Author: Enric Garcia Torrents, MSc, PhD candidateMedical Anthropology Research Center, Universitat Rovira i Virgili The main role of a medical anthropologist is to study human health, the whole range of actual and potential care systems, and the ways in which biocultural adaptations emerge, succeed or fail from a transdisciplinary, multidimensional and ecological perspective. We contemplate the processes and situations from within and outside the limits of our own culture, and even our own civilisation, from a long-range evolutionary perspective to the minute details of small social networks analysis. We dive deep into the complexities and repeating patterns with a skill set and toolkit as sharp, in many cases, as that of a fully trained physician-scientist, being able to engage constructively in laboratory, fieldwork and clinical practice. “It is possible that the greatest contribution that anthropology can make will be to keep men's imaginations open, as they tend to let the predictable hardware coerce the form of the software.” Space medical anthropologists, on the other hand, are bound to take the whole field of medical anthropology one step further and even beyond, daring to question what it is to be a healthy human today, what it may mean to be so tomorrow, and indeed, what the near future might bring, depending on what we decide to do at this point in history. Most importantly, space medical anthropologists work on how to achieve this healthy state by skillfully setting the stage here and now, maximising humanity’s chance for a sustainable way onward to the stars. As for myself, nowadays I'm a scholar working as a doctoral candidate at a Medical Anthropology Research Center while undertaking medical studies (MD-PhD student-researcher, second and third year within the dual degree). I have previous academic background in neuroscience and smart systems, and currently a contract from the Spanish Ministry of Universities to undertake research on mental health and clinical decision making for choosing the best possible treatments for each individual, funded from a future professor’s training programme. My work on space medical anthropology is rather narrow, focusing almost exclusively on figuring out the best ways for people to withstand extreme experiences without losing mental acuity, exploring optimal solutions to boosting cognitive performance, resilience and overall wellbeing in situations of acute and profound distress.
Cardiopulmonary resuscitation (CPR) is a well-established part of basic life support (BLS), having saved countless lives since its first development in the 1960s. External chest compressions (ECCs), which form the main part of BLS, must be carried out until Advanced Life Support can begin. It is essential that ECCs are performed to the correct depth and frequency to guarantee effectiveness. The absence of gravity during spaceflight means that performing ECCs is more challenging. The likelihood of a dangerous cardiac event occurring during a space mission is remote, however, the possibility does exist. Nowadays, the selection process for space missions considers individuals at ages and with health standards that would have prohibited their selection in the past. With increased age, less stringent health requirements, longer duration missions and increased physical labour, due to a rise in orbital extravehicular activity, the risk of an acute life-threatening condition occurring in space has become of greater concern. The advent of space tourism may even enhance this possibility, with its popularity set to rise over the coming years as private companies test their new technology. Therefore, space scientists and physicians will have a greater responsibility to ensure space travellers, whether professional astronauts or space tourists, are adequately trained and familiarised with extraterrestrial BLS and CPR methods. Recently, work has been undertaken to develop methods of basic and advanced life support in microgravity and hypogravity, and several CPR techniques have been developed and tested. This blog presents one of these, the Evetts-Russomano MicroG CPR Method. Evetts-Russomano MicroG CPR Method In the Evetts-Russomano (ER) method, the rescuer can respond immediately, as it requires no additional CPR equipment/medication or the use of a restraint system. To assume the position, the rescuer places their left leg over the right shoulder of the patient and their right leg around the patient’s torso, allowing their ankles to be crossed approximately in the centre of the patient’s back; this is to provide stability and a solid platform against which to deliver force, without the patient being pushed away. From this position, chest compressions can be performed while still retaining easy access to perform ventilation. When adopting the ER CPR method, the rescuer must be situated in a manner that also allows sufficient space on the patient’s chest for the correct positioning of their hands to deliver the chest compressions. Extraterrestrial CPR simulation The main difference between extraterrestrial and terrestrial CPR is the strength of the gravitational field. In microgravity, patient and rescuer are both essentially weightless. When thinking about the technique of terrestrial CPR, with the rescuer accelerating their chest and upper body to generate a force to compress the patient’s chest, it is obvious that this cannot work in microgravity without significant aids. To this end, the ER CPR method has been developed using a ground-based microG simulation, during parabolic flights, and subsequently tested under-water! Video credits: Ground-based MicroG Simulation (land) = Space Researcher Lucas Rehnberg, MD (MicroG Center PUCRS, Brazil) Parabolic Flight MicroG Simulation (air)= Researchers = Thais Russomano, Simon Evetts, Lisa Evetts & João Castro (ESA 29th Parabolic Flight Campaign, Bordeaux, France) Underwater MicroG Simulation (water) = Sea King Dive Center, Chengdu, China - Instructor Gang Wei; Chinese Space First Responder & Space Researcher/Instructor Chris Yuan A project of InnovaSpace, PECA and Guangxi Diving Paradise Club, China Free Resource: Extraterrestrial CPR and Its Applications in Terrestrial Medicine
Authors: Thais Russomano, Lucas Rehnberg In book: Resuscitation Aspects, Ed: Theodoros Aslanidis Publisher: IntechOpen 2017 See Download Link at https://www.innovaspace.org/chapters.html Os autores são membros do time da InnovaSpace e possuem vasta experiência profissional em medicina de aviaçāo e fisiologia aeroespacial - ensino, pesquisa e inovaçāo.  O Problema Emergências médicas durante voos comerciais de curta ou longa duração, nacionais ou internacionais, estão se tornando cada vez mais comuns. Isso se deve a fatores já conhecidos, como a expansão da indústria da aviação, a popularização dos voos comerciais e a maior diversidade do perfil do viajante, incluindo passageiros idosos, portadores de doenças crônicas ou usuários de medicações. Junta-se aqui o próprio ambiente de cabine, que impõe, por exemplo, o estresse da hipóxia hipobárica, dos disbarismos pela expansão de gases de cavidades corporais, da exposição ao ar frio e seco, a ruídos, a vibrações e a acelerações, da alteração do ciclo circadiano, da fadiga e da imobilidade. Esses fatores afetam pouco ou nada os organismos sadios, mas podem ser danosos em diferentes graus ao passageiro idoso e/ou portador de doenças crônicas. A Situação Exemplo 1 – Uma avaliação clínica ou pré-operatória - Quando o motivo de uma consulta médica é uma avaliação clínica ou pré-operatória, deve-se questionar e considerar vários aspectos durante a anamnese, o exame físico e os exames laboratoriais, para se chegar a melhor decisão clínico-cirúrgica possível, reduzindo ao máximo possíveis eventos adversos, minimizando desfechos não desejados e otimizando a segurança do paciente no voo. Assim, uma pergunta não deve faltar na anamnese - “Existe o plano de uma viagem aérea num futuro próximo?”. Para que esse questionamento, no entanto, produza um impacto positivo na tomada de decisão, é mandatório que o médico assistente detenha conhecimento sobre as condições estressantes do ambiente de cabine de uma aeronave e as condições do passageiro enfermo, objetivando discutir o planejamento de um voo seguro ou até mesmo o cancelamento ou postergação do mesmo. Exemplo 2 – Médico a bordo? – Incidentes médicos com passageiros em voos comerciais vêm se tornando mais comuns. No entanto, o ambiente de cabine e os recursos médicos disponíveis a bordo de aeronaves são quase sempre de total desconhecimento dos médicos que se tornam voluntários no atendimento a um passageiro durante um voo comercial. Sistemas de auxílio às tripulações a ao médico voluntário incluem o uso da saúde digital e da telemedicina, as quais, nem sempre estão disponíveis para orientação num incidente médico a bordo. Ainda, muitos casos poderiam ter sido evitados, se, durante a avaliação pré-voo por parte do médico clínico, especialista ou cirurgião, fosse incluído na anamnese do paciente questionamentos relativos a planos de viagens de avião. A Solução A InnovaSpace vem adovagar em favor do ensino da Medicina de Aviação e da Fisiologia Aeroespacial na formação de estudantes de faculdades de medicina, através da inserção de uma série de aulas constituindo disciplinas curriculares novas ou integrando disciplinas já existentes no currículo acadêmico. Esta iniciativa é apoiada pelas Sociedade Brasileira de Medicina Aeroespacial (SBMA) e
Sociedade Portuguesa de Medicina Aeronáutica (SMAPor) The InnovaSpace team welcome this contribution from Prof. Ganapathy and we send huge congratulations to the team at Apollo Telehealth Services on achieving ISO 13131 certification - a great achievement! Prof. Krishnan GanapathyPast President, Telemedicine Society of India & Neurological Society of India | Hon Distinguished Professor The Tamilnadu Dr MGR Medical University | Emeritus Professor, National Academy of Medical Sciences | Formerly Adjunct Professor IIT Madras & Anna University | Director Apollo Telemedicine Networking Foundation &, Apollo Tele Health Services | URL: www.kganapathy.in  December 10th 2021 was indeed a Red letter day for Indian Telehealth. On this day the ISO 13131-2021, certification for Telehealth Services was obtained for the first time anywhere, by Apollo Telehealth Services. This brief note points out the necessity for raising the bar and setting high standards, so that the world will strive to achieve India class. For decades, Telemedicine/Telehealth services were not centre stage in the healthcare delivery system. COVID-19 changed this. The world has now accepted that the forced lockdown- enforced acceptance of Remote Health Care - will become the new normal even after the pandemic is de notified. Universal acceptance increases the responsibility of all health care providers deploying technology, to ensure constant high quality while bridging the urban-rural health divide. Quality is never an accident. It is always the result of deliberate intention, sincere effort, intelligent direction and skilful execution. Though Henry Ford opined that quality means doing it right when no one is looking, in the real world this is difficult to implement. ISO certification ensures that “Big Brother” is watching all the time. The necessity for re certification is like the Sword of Damocles hanging above us. However, it drives home the message that Quality is everyone’s responsibility at all times and not during the audit alone. One has to keep running to stay where you are. To maintain the initial global recognition, maintaining quality needs to become a habit, a unique opportunity to transform one’s DNA if necessary!! Success is the sum of small efforts, repeated day-in and day-out. Standardising systems, processes, documentation and re documentation alone will ensure providing quality remote healthcare for anyone, anytime anywhere.
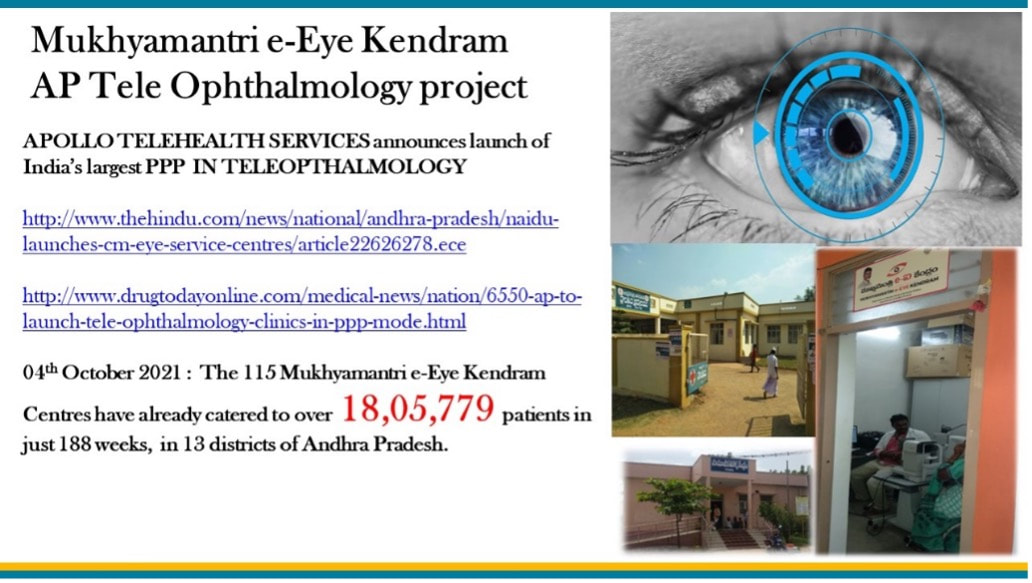
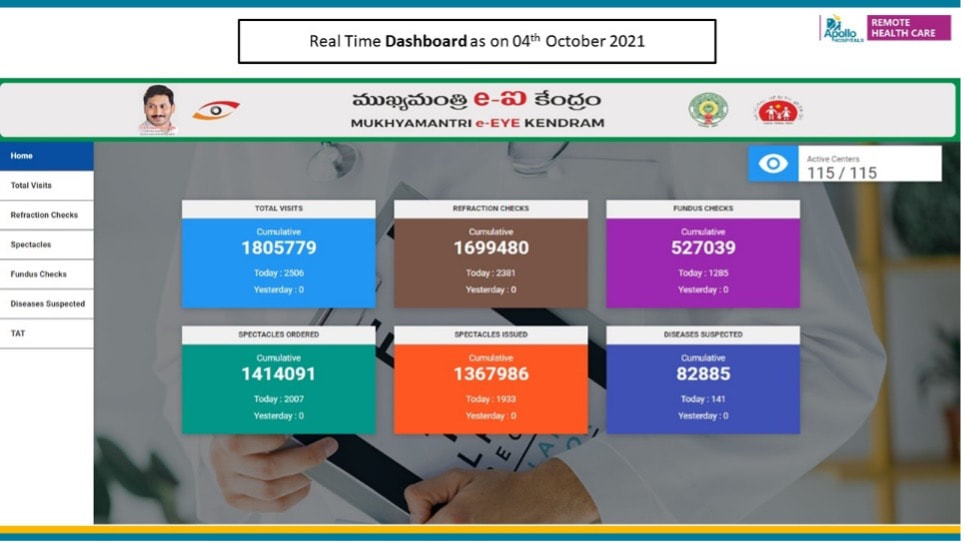
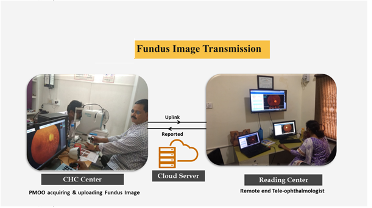
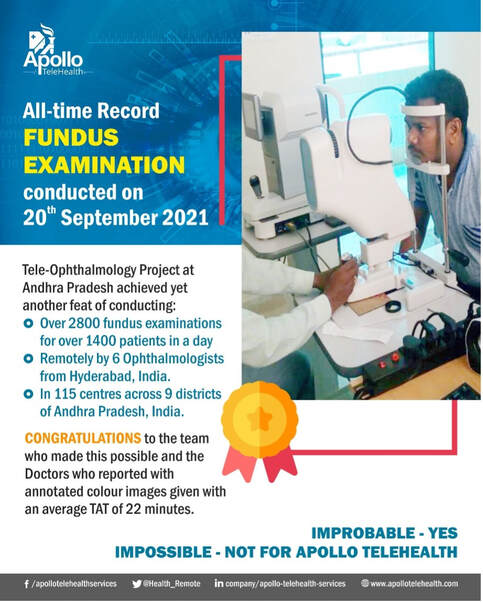
International Organization for Standardization (ISO) – An OVERVIEW The, International Standards Organization, TC 215 Health Informatics Committee developed a Technical Specification, ISO/TS 13131 Telehealth services, based on a risk and quality management approach. This standard supports healthcare planning, service and workforce planning, organization responsibilities, financial and IT management. ISO was established in 1947 in Geneva, Switzerland. An Independent, non-governmental international organization it develops standards that are recognized and respected globally. It brings experts together to improve quality and provide world-class healthcare services. Experts are from 166 national standard bodies. ISO standards are developed by various advisory groups. Presently ISO has 255 technical committees, 515 subcommittees, and 2498 working bodies. Since 1947, ISO’s technical experts have created more than 18,800 standards for all possible business. ISO standards ensure that administration and product/workflow systems are carried out legally, safely and effectively. ISO technical experts have developed several assessment protocols to ensure that certified organizations apply these guidelines in their workplace. The approved protocols aid organisations to ensure that their frameworks, devices and workforce are actually in compliance with ISO standards. ISO 13131 provides recommendations on guidelines for Telehealth services deploying Information and Communication Technology (ICT) to deliver quality healthcare services. Prof. Krishnan GanapathyDistinguished Professor at Tamilnadu Dr MGR Medical University, India & a WHO Digital Health Expert. Past President of the Telemedicine Society of India, Neurological Society of India, and Indian Society for Stereotactic & Functional Neurosurgery. Member of the Board of Directors of Apollo Telemedicine Networking Foundation and Apollo Telehealth Services, and InnovaSpace Advisory Board member - Visit: drkganapathy.com Distance is Meaningless and Geography has become History - paraphrasing Star Trek's Captain Kirk, played by William Shatner (who just flew on a sub-orbital flight on 12th October 2021 at the age of 90 years) and going where No man has ever gone before is not the prerogative of the elite 600 plus astronauts who have left the confines of Terra Firma. In an activity that would have seemed like science fiction just a few years ago, 30 Retinal Specialists have been peering into 2800 eyes a day from a distance of 175 to 350 km, and ensuring that a digitally-signed colour-coded annotated fundus report (assisted with semi-automated diagnosis) is physically provided to each villager within 25 minutes. And this has now been happening daily for the last 43 months, in a service that the beneficiary gets totally free, thanks to a Public-Private Partnership project. An acute shortage of eye care personnel in rural India results in millions unnecessarily developing visual impairment. Early diagnosis and initiation of corrective measures remotely could be a major public health initiative, whereby the Government fills a large void by providing free, quality eye care services, including spectacles, to the community. The Andhra Pradesh Government has now been implementing the “Mukhyamantri e-Eye Kendram-MeEK (http://enethraap.phc.ind.in/) program since 1st February 2018. This tele-ophthalmology service is one of the largest Public-Private Partnership projects. In just 43 months 1.7 million patients have had their eyes checked in 115 Eye centres located in 9 districts of Andhra Pradesh, a state in southern India. A total of 1.4 million spectacles have been ordered following 1.7 million refraction checks! The operational challenges in providing “customer delight” to 2000 + people every day in so many rural centres is indeed a humongous task. Some 0.5 million fundus examinations have been performed remotely and abnormal pathology detected in 83,000 cases, including Diabetic Retinopathy, Hypertensive Retinopathy, Glaucoma and other pathologies. Continuous quality control and ensuring constant compliance and adherence to strict deliverables is in the DNA of the entire fantabulous team who continued to work even during the height of the pandemic. Obsession with perfection - where failure is not an option, making the impossible possible - these are the stuff of which astronauts and the entire extended team remotely connected with space exploration are made up of. Who knows, perhaps this project is a good recruiting ground for ISRO, ESA and NASA – after all there are a lot of similarities !!
Final blog from ESA-sponsored Dr Stijn Thoolen, from his series written while spending 12 months at the Concordia research station in Antarctica. Catch up on the rest of his fascinating blogs by following the links: Part 1, Part 2, Part 3, Part 4, Part 5, Part 6, Part 7, Part 8, Part 9, Part 10, Part 11, Part 12 Dr Stijn Thoolen Medical Research Doctor, Concordia Research Station, Antarctica L’Astrolabe icebreaker, December 15, 2020 Sunlight: 24 hours a day, but tomorrow, as we head further north, it will set again Temperature: Around 0 °C Mood: not sure how to describe it today. I am excited and just feel very lucky. It’s midnight. Since our departure some hours ago the sun has steadily moved towards the horizon behind us, and it has started to paint the sky in colours that make me think of winter again. Huge icebergs are slowly passing by, and every once in a while there is a bunch of curious penguins waving us goodbye from their ice floe. Not much earlier I saw a seal chilling, and there have been whales too. In the very far distance I can still recognise the enormous ice mass on which we have been living our lives the past year. It’s my last view of the Antarctic, and it’s perfect. Standing here alone on the deck of the Astrolabe surrounded by all this beauty I have found myself a special opportunity to appreciate once more where the #$%!! (beep) we have been all this time. It is just so different there on top of the ice, so far away from the rest of the world, that as we are slowly being re-introduced to civilisation I am having a hard time believing it actually happened. With all the changes that we have gone through lately and with all the new impressions time has gone fast, and it has made Concordia feel like a distant, almost unrealistic memory. Like ages ago, even though it has only been eight days since we left… It started when the ‘orange and fat’ people (and kiwis!) arrived at Concordia about a month ago. With the start of the summer campaign our winterover isolation had come to an abrupt end, and I remember the calm, safe and familiar environment of the ESA lab feeling surprisingly pleasant after some intense hours of new social interactions. As a positive summer energy took hold of the station and fresh ESA MD Nick gradually took over the lab, there was no way for me to hide anymore. Unavoidable steps out of our rigid routines, but at that ‘c’est l’Antarctique’ rate of change that isn’t always easy to keep up with.
Our departure from Concordia last week was much the same. Emotionally numb from a lack of realisation of what was happening (or a lack of sleep the night before…) it just passed by so quickly, and surprisingly smooth. I said my goodbyes without any affection for the tears around me. I gave the station a good last look for the sake of memory. But when the plane started accelerating for lift-off, suddenly that strong desire came up to make it stop and bring me back safely into the station. Apparently part of me wasn’t ready to leave at all. Too big steps too quickly I guess, but lucky for me there were pilots taking care of that... A penultimate blog from ESA-sponsored Dr Stijn Thoolen, from his series written while spending 12 months at the Concordia research station in Antarctica. Enjoy the rest of his fascinating blog series by following the links: Part 1, Part 2, Part 3, Part 4, Part 5, Part 6, Part 7, Part 8, Part 9, Part 10, Part 11 Dr Stijn ThoolenMedical Research Doctor, Concordia Research Station, Antarctica Concordia, November 29, 2020 Sunlight: 24 hours Windchill temperature: -45 °C Mood: positive, focused Today is Sunday. We are on full summer campaign steam for two weeks now. There are about 40 people occupying the station, but today nobody works. Instead, I am wearing three layers on my legs, five on my torso, two pairs of socks, neck warmer, two balaclavas, hat, goggles, glove liners, mittens, radio, and of course my running shoes. I prepared two-and-a-half litres of isotone sport drink and extra electrolyte tablets against the dry desert atmosphere. Extra goggles for when my visor fogs from sweat that cools off in the freeze. Battery-powered heated gloves, air-activated hand- and feet warmers as well as another pair of shoes for when my body becomes unable to pump sufficient blood to my fingers and toes to keep them warm. Bananas and chocolate bars accommodating high energy demands at this altitude and these temperatures. Spare radio battery to make sure I maintain contact with the station. Tape for whatever unforeseen circumstances, and four volunteers and a skidoo standing by to support me with whatever I request. Today I am going to run a marathon. I guess I can sometimes be a bit of a dreamer. Not necessarily in the sense that I tend to lose touch with the world around me in order to float around in some self-invented realm in a galaxy far, far away (no worries, I do that too sometimes), but I do like to fantasise about doing things that are commonly perceived as unachievable. Or at least to say a challenge. Then afterwards I see myself devoting quite some time towards realising (some of) such ideas, because it makes me feel good. Contradicting, right? Well, I have to admit I sometimes do find myself wondering why the … I got myself in an awkward position again, but overcoming a challenge in the end always makes me feel proud, and most importantly the experience that comes with it makes me learn.
As I have probably mentioned in all my previous blogs (hope I am not starting to bore you), I strongly believe that pushing yourself into an unknown (decide for yourself how) and leaving your comfortable space can broaden your horizon. We can allow ourselves to understand the world around us from new perspectives, and see new ways of tackling the difficulties that life will offer us. In that sense, I guess it can make us more resilient. Isn’t that exciting? It is this curiosity that made me come to Antarctica in the first place, and enjoy the winterover experience that is often said to bring positive psychological impact to those who are able to overcome the challenge of being far from home in isolation and confinement. Learning from terrestrial healthcare: 3 ways to get medical autonomy for deep space travel13/5/2021
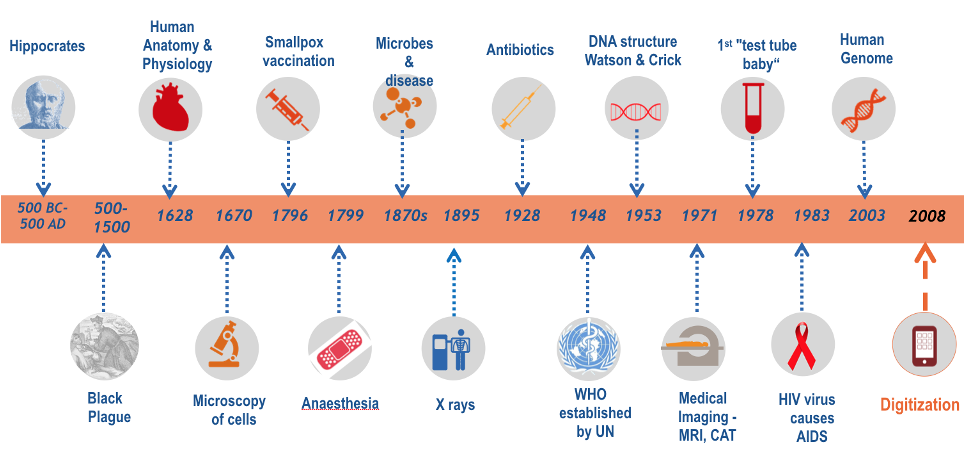
Jules LanceeBiomedical engineer, with a focus on emerging technologies and their role in the changing world of healthcare. He explores how they will impact the care delivered to patients, but is also equally interested in how they could benefit the future of long-term spaceflight. He believes both questions are opportunities for collaboration and inspiration!  SpaceX Starship landing SpaceX Starship landing How would you deal with physical and mental health needs on a three-year round-trip to Mars? Those are questions I often think about and I would like to take you on a tour of solutions already out here on Earth, that might benefit those first astronauts to the Red Planet. Last week SpaceX performed another successful test of its Starship. The Starship is designed to eventually bring as many as a 100 people to Mars per flight. We’ve seen many recent plans for human spaceflight, both commercial and non-commercial and it’s about right to say that humankind will go on more and longer duration space missions. A lot of engineering research is going into the development of rockets and other technological advancement, but just as important as getting there, will be getting there alive and healthy! That’s not a trivial problem: Especially when we will go on deep space missions to Mars and beyond we will run into some basic limitations. There will be communication delays, we will have limited medical equipment on board due to limitations in mass, volume and electricity, and limited medical skills. A doctor can come along, but the doctor can also become sick, and of course, emergency evacuation to Earth will no longer be an option. Therefore, we will need a sense of medical autonomy for those astronauts on the go. We will send the most healthy human beings on such a mission, but a 3-year trip is a long time to stay healthy in the extreme environment of outer space. If not physical problems, then also psychological issues can become a risk to the success of the mission, which the crew themselves will need to deal with. In this quest for medical autonomy, I argue, we can learn from trends in healthcare and healthcare innovation on Earth, so let’s shortly take a trip back to Earth. In this short overview of the history of healthcare, a lot has happened since Hippocrates worked out the oath for medical professionals. None of the developments shown however, were as fundamental as the last one, the advent of digital health technologies. By becoming digital, solutions for healthcare have become smaller, faster, cheaper and in many cases, smarter. Solutions are leveraging Artificial Intelligence, Virtual and Augmented Reality, blockchain, voice recognition and 3D printing. These are just some of the technologies that are impacting healthcare.
As a result of this impact, we see various shifts in healthcare, going from a reactive system to more preventive care and from a one-size-fits-all-healthcare to precision medicine. Most importantly, however, you see a shift in power. The relationship between the doctor and his or her patient is changing from a more dependent relationship, into a partnership, in which the patient is empowered with technology, to take care of his/her own health or medical issues. In other words, terrestrial patients are becoming more autonomous when it comes down to their health and care. It is this change, that is also needed for astronauts on their way to Mars. A different relationship between astronauts and their doctors in mission control is needed and this can be achieved, by leveraging new health technologies. Here are 3 terrestrial examples: As ESA-sponsored Dr Stijn Thoolen comes closer to the end of his year at the Concordia research station in Antarctica, he begins to reflect on his experiences of the last year and the journey homewards. Enjoy the rest of his fascinating blog series by following the links: Part 1, Part 2, Part 3, Part 4, Part 5, Part 6, Part 7, Part 8, Part 9, Part 10 Dr Stijn ThoolenMedical Research Doctor, Concordia Research Station, Antarctica Concordia, October 4, 2020 Sunlight: about 14 hours per day Windchill temperature: -85 °C Mood: excited, but there is a pinch of nostalgia. Already… It’s 1:00 AM. I am lying outside on the roof, together with Ines (glaciologist), Elisa (cook) and Andrea (vehicle mechanic). There is a full moon shining on us, and Mars is right next to it. I am not much of an astronomer, but its bright color stands out so clearly from all the other celestial objects that even I can recognize it instantly as the Red Planet. Looking to the southwest I see Jupiter and Saturn. Also pretty hard to miss. Usually that is where I find the Milky Way, but there is too much light now, even at this hour. An amber color brightens the horizon, beyond which I now realize again there are just so many miles of ice (something easily taken for granted here, but thinking back to that inbound flight to Concordia last year does the trick) separating us from the rest of the world. In front of it all, I look at the frosty metal bars, which always looked so surrealistic to me when I saw pictures of them back home. They have gone through winter as well…
The return of the sun was cool. ‘Here comes the sun’ (you know, that one from the Beatles) was heard all over the station while we impatiently and excitedly tried to catch a first glimpse of it mid-August. Since that moment the skies have become more and more blue, and the snow more and more bright. I have experienced the gradual return of daylight over the past weeks with a positive and fresh feeling, and a sense of anticipation has started to take hold of the station. Who are the people who will replace us? What are our plans after Concordia? I remember myself some weeks ago, lying in exactly the same position as I am right now, outside against a snow dune, sheltered from the wind and with a pleasant -50 degrees Celsius (I realize this perception must be taken relatively…), alone, and just letting the sunshine touch my face again. A special moment, that reminded me of how pleasant summer conditions are going to be.
We welcome back helicopter flight physician Dr Alessandro Forti, as he recounts the true story of an incredible mountain rescue in the Dolomites. We never truly know when we wake up each morning if this could be our last day of life - we assume that all will be well - as did a keen mountaineer in Italy, whose life unexpectedly hung in the balance and in the responsible hands of a Helicopter Emergency Medical Service team with a Lucas device! Do also take a look at Alessandro's previous blog, which began his dream to work in the rescue services. We describe here a case of full neurologic recovery from accidental hypothermia with cardiac arrest, which involved the longest reported duration of mechanical cardiopulmonary resuscitation (CPR) and extracorporeal life support (8 hours, 42 minutes). A 31-year-old man experienced a witnessed hypothermic cardiac arrest with a core temperature of 26C° (78.8F) during a summer thunderstorm on the vertical wall of the Marmolada mountain in the Dolomites, Italy (Figure 1), in the late afternoon on a summer day (day 0). The trapped climber was secured on the wall without any form of waterproof clothing and reportedly had already lost consciousness in the few minutes it took his companion to reach him. The companion signalled for help, using a light on his smartphone device directed toward a nearby mountain hut. The local helicopter emergency medical system was called (7:20 PM) (Figure 2). 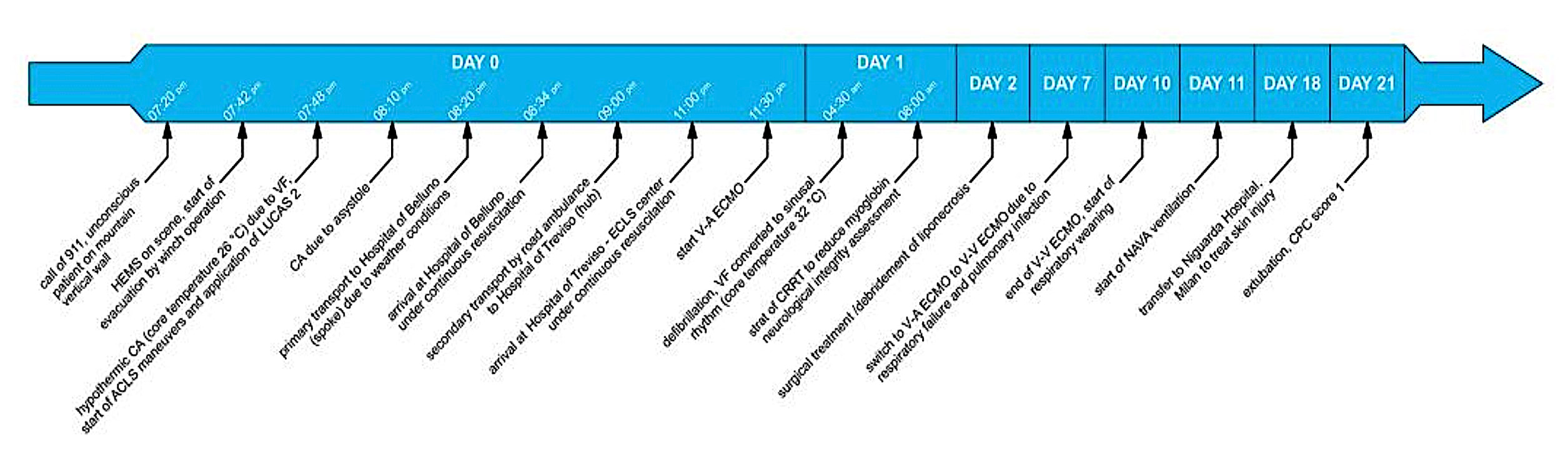 FIGURE 2: Course of treatment. HEMS, hospital emergency medical system; CA, cardiac arrest; VF, ventricular fibrillation; ACLS, advanced cardiac life support; ECLS, extracorporeal life support; CRRT, continuous renal replacement therapy; NAVA, neurally adjusted ventilator assist; CPC, cerebral performance category  LUCAS 3 system maintaining chest compressions LUCAS 3 system maintaining chest compressions A physician-staffed helicopter reached the scene at 7:42 PM, and the unconscious patient was immediately evacuated with a 30-m winch operation. The helicopter landed nearby; the initial cardiac rhythm was a low-voltage ventricular fibrillation (7:48 PM). Resuscitation manoeuvres started immediately with manual CPR, followed after a few seconds by an electrical shock (200 J biphasic); mechanical CPR was started after one complete cycle of manual resuscitation. CPR was continued with a mechanical chest compression device (LUCAS 3; Physio Control, Redmond, WA); initial end-tidal carbon dioxide (ETCO2) level ranged between 14 and 22 mm Hg. At 8:20 PM, the patient was transferred by helicopter under continuous mechanical CPR to the spoke Hospital of Belluno, Italy (43 km; arrival at 8:34 PM), as a direct flight to the hub Hospital of Treviso, Italy, was impossible because of the darkness. On arrival, the patient’s core temperature was stable (26.6C° [79.9F]) and cardiac output under continuous CPR was considered sufficient (ETCO2 22 mm Hg); therefore, in accordance with the local protocol for refractory hypothermic cardiac arrest, the patient was transferred to a road ambulance and transported to the hub hospital (Treviso, Italy; 83 km) under ongoing mechanical CPR; meanwhile, the extracorporeal life support team was alerted. After the patient’s arrival (11 PM), venous-arterial extracorporeal membrane oxygenation (ECMO) was commenced (11:30 PM). Core temperature (esophageal) was 26.1C°. On day 10, there was a partial recovery of the ventricular function (left ventricular ejection fraction 40%) and ECMO was removed. On day 21, the patient was extubated; cerebral performance category score was 1, with only mild retrograde amnesia at day 28. Three months and 10 days after the accident, the patient left the rehabilitation unit and resumed normal daily life activities, with only minimal impairment of short-term verbal memory. After one year the patient and the companion return to the place of the accident and with an US film factory and Stryker filmed a documentary about this event. |
Welcometo the InnovaSpace Knowledge Station Categories
All
|
UK Office: 88 Tideslea Path, London, SE280LZ
Privacy Policy I Terms & Conditions
© 2024 InnovaSpace, All Rights Reserved























 RSS Feed
RSS Feed