Author: Prof K GanapathyDirector Apollo Telemedicine Networking Foundation, Apollo Tele Health Services | Distinguished Visiting Professor IIT Kanpur | Distinguished Professor The Tamilnadu Dr MGR Medical University | Emeritus Professor National Academy of Medical Sciences  5G is the fifth generation of wireless communication technology, promising faster data transfer speeds, lower latency (round trip latency >10 milliseconds), increased network capacity (1 million devices per sq km), 99.999% network reliability and battery life of up to 10 years for IoT devices. There is considerable hype in the media that deployment of 5G will revolutionize healthcare by enabling new medical applications and improving existing ones. Using Edge computing, 5G Data can be processed closer to where it is generated. IoMT (Internet of Medical Things) devices generate huge amounts of data. Cloud computing can provide the necessary infrastructure to process and analyze this data. Faster transmission of data will enable more efficient storage in the cloud. Accessing more bandwidth and computing resources, and providing infrastructure to enable scalability will now be less problematic. No doubt clarity of images transmitted will be better and the immersive experience in video conferencing will be an all-time high. Mammograms, CT, MRI, and ultrasound images generate large amounts of data. High-speed transfer and processing will save a few minutes. Onboard cameras, camera-based Headgear, and ‘Body Cams’ for paramedics can transmit patient data to hospitals in real-time using ultra-fast and low-latency 5G connected ambulances, with medical equipment, patient monitoring applications and telemetry devices that ensure excellent pre-hospital management. 5G can facilitate real-time control of medical robots, enabling precise and safe interventions in performing complex procedures. 5G enables faster and more efficient data transfer, facilitating clinical trials and drug development, as these require the collection of large amounts of data from multiple sources.
Author: Prof. K. GanapathyHon Distinguished Professor The Tamilnadu Dr MGR Medical University; Emeritus Professor, National Academy of Medical Sciences; Past President, Telemedicine Society of India & Neurological Society of India; Director Apollo Telemedicine Networking Foundation & Apollo Tele Health Services, India ABSTRACT: Introduction: Metaverse is the augmented virtual world formed by convergence of virtual and physical space. Users interact within this created world, meeting each other virtually, immersing themselves in performing virtual activities, which subsequently could lead to real experiences. Conventionally, the healthcare “industry” is conservative in deploying future ready technology. Aims and Objectives: This overview discusses the untapped potential of metaverse applications in healthcare from a clinician’s perspective. Bereft of technical jargon, the article points out the advantages, disadvantages, limitations, and challenges in actual deployment of the metaverse in clinical practice in the real world. The exponential transformation occurring in this area is highlighted. The highly technical literature is simplified for easier comprehension. Findings: Clinical applications, use of the metaverse in training, education, and augmenting telehealth consultations, in an immersive milieu, is discussed. Direct “in-person” interaction with digital products and solutions will be a new experience for a healthcare provider and the beneficiary. The role of digital twins is illustrated. Consultation process and various clinical applications in the metaverse are outlined. Technology‑enabled futuristic training and education is discussed. Conclusion: Demonstrating significant improvement in healthcare outcomes using the metaverse will be difficult to prove. This alone will ultimately lead to the development of a business model, insurance reimbursement and behavioral modification necessary for accepting and using, a hitherto unused method in patient care. Keywords: Augmented reality and healthcare, blockchain and healthcare, metaverse and healthcare, virtual reality and healthcare The full article can be read and freely downloaded following this LINK
Os autores são membros do time da InnovaSpace e possuem vasta experiência profissional em medicina de aviaçāo e fisiologia aeroespacial - ensino, pesquisa e inovaçāo.  O Problema Emergências médicas durante voos comerciais de curta ou longa duração, nacionais ou internacionais, estão se tornando cada vez mais comuns. Isso se deve a fatores já conhecidos, como a expansão da indústria da aviação, a popularização dos voos comerciais e a maior diversidade do perfil do viajante, incluindo passageiros idosos, portadores de doenças crônicas ou usuários de medicações. Junta-se aqui o próprio ambiente de cabine, que impõe, por exemplo, o estresse da hipóxia hipobárica, dos disbarismos pela expansão de gases de cavidades corporais, da exposição ao ar frio e seco, a ruídos, a vibrações e a acelerações, da alteração do ciclo circadiano, da fadiga e da imobilidade. Esses fatores afetam pouco ou nada os organismos sadios, mas podem ser danosos em diferentes graus ao passageiro idoso e/ou portador de doenças crônicas. A Situação Exemplo 1 – Uma avaliação clínica ou pré-operatória - Quando o motivo de uma consulta médica é uma avaliação clínica ou pré-operatória, deve-se questionar e considerar vários aspectos durante a anamnese, o exame físico e os exames laboratoriais, para se chegar a melhor decisão clínico-cirúrgica possível, reduzindo ao máximo possíveis eventos adversos, minimizando desfechos não desejados e otimizando a segurança do paciente no voo. Assim, uma pergunta não deve faltar na anamnese - “Existe o plano de uma viagem aérea num futuro próximo?”. Para que esse questionamento, no entanto, produza um impacto positivo na tomada de decisão, é mandatório que o médico assistente detenha conhecimento sobre as condições estressantes do ambiente de cabine de uma aeronave e as condições do passageiro enfermo, objetivando discutir o planejamento de um voo seguro ou até mesmo o cancelamento ou postergação do mesmo. Exemplo 2 – Médico a bordo? – Incidentes médicos com passageiros em voos comerciais vêm se tornando mais comuns. No entanto, o ambiente de cabine e os recursos médicos disponíveis a bordo de aeronaves são quase sempre de total desconhecimento dos médicos que se tornam voluntários no atendimento a um passageiro durante um voo comercial. Sistemas de auxílio às tripulações a ao médico voluntário incluem o uso da saúde digital e da telemedicina, as quais, nem sempre estão disponíveis para orientação num incidente médico a bordo. Ainda, muitos casos poderiam ter sido evitados, se, durante a avaliação pré-voo por parte do médico clínico, especialista ou cirurgião, fosse incluído na anamnese do paciente questionamentos relativos a planos de viagens de avião. A Solução A InnovaSpace vem adovagar em favor do ensino da Medicina de Aviação e da Fisiologia Aeroespacial na formação de estudantes de faculdades de medicina, através da inserção de uma série de aulas constituindo disciplinas curriculares novas ou integrando disciplinas já existentes no currículo acadêmico. Esta iniciativa é apoiada pelas Sociedade Brasileira de Medicina Aeroespacial (SBMA) e
Sociedade Portuguesa de Medicina Aeronáutica (SMAPor) The InnovaSpace team welcome this contribution from Prof. Ganapathy and we send huge congratulations to the team at Apollo Telehealth Services on achieving ISO 13131 certification - a great achievement! Prof. Krishnan GanapathyPast President, Telemedicine Society of India & Neurological Society of India | Hon Distinguished Professor The Tamilnadu Dr MGR Medical University | Emeritus Professor, National Academy of Medical Sciences | Formerly Adjunct Professor IIT Madras & Anna University | Director Apollo Telemedicine Networking Foundation &, Apollo Tele Health Services | URL: www.kganapathy.in  December 10th 2021 was indeed a Red letter day for Indian Telehealth. On this day the ISO 13131-2021, certification for Telehealth Services was obtained for the first time anywhere, by Apollo Telehealth Services. This brief note points out the necessity for raising the bar and setting high standards, so that the world will strive to achieve India class. For decades, Telemedicine/Telehealth services were not centre stage in the healthcare delivery system. COVID-19 changed this. The world has now accepted that the forced lockdown- enforced acceptance of Remote Health Care - will become the new normal even after the pandemic is de notified. Universal acceptance increases the responsibility of all health care providers deploying technology, to ensure constant high quality while bridging the urban-rural health divide. Quality is never an accident. It is always the result of deliberate intention, sincere effort, intelligent direction and skilful execution. Though Henry Ford opined that quality means doing it right when no one is looking, in the real world this is difficult to implement. ISO certification ensures that “Big Brother” is watching all the time. The necessity for re certification is like the Sword of Damocles hanging above us. However, it drives home the message that Quality is everyone’s responsibility at all times and not during the audit alone. One has to keep running to stay where you are. To maintain the initial global recognition, maintaining quality needs to become a habit, a unique opportunity to transform one’s DNA if necessary!! Success is the sum of small efforts, repeated day-in and day-out. Standardising systems, processes, documentation and re documentation alone will ensure providing quality remote healthcare for anyone, anytime anywhere.
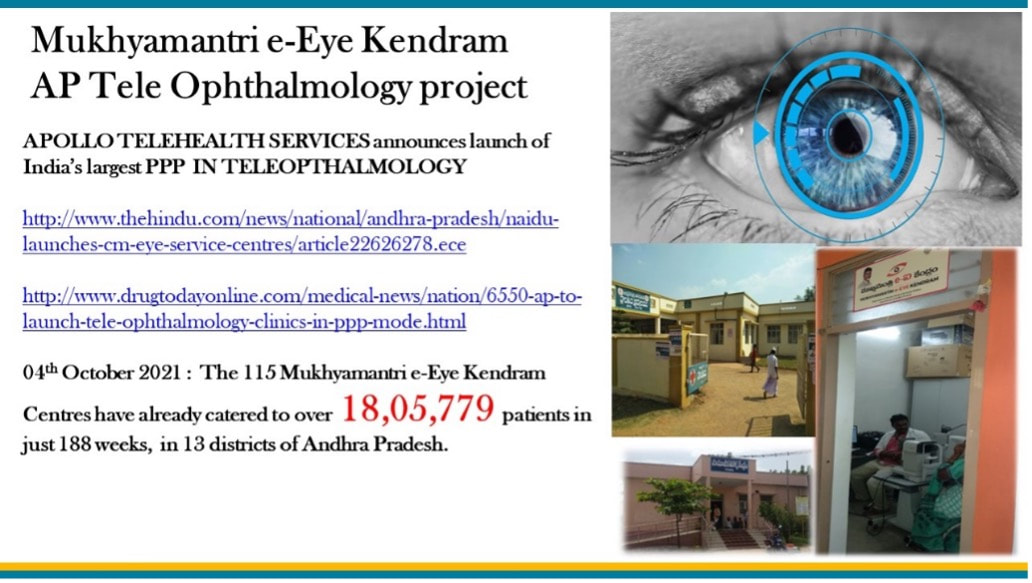
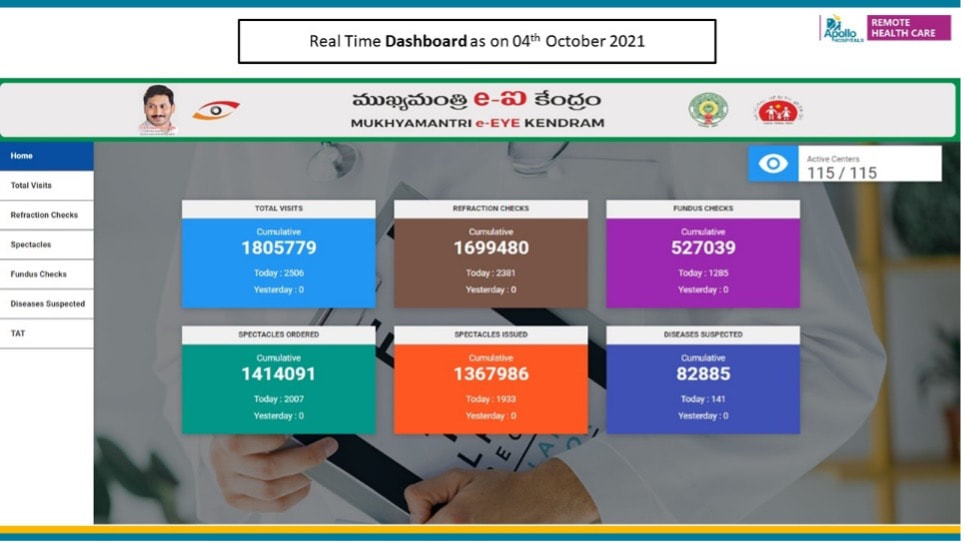
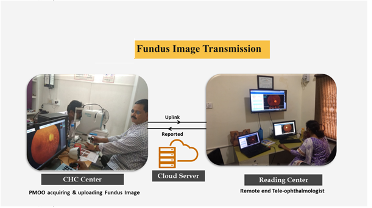
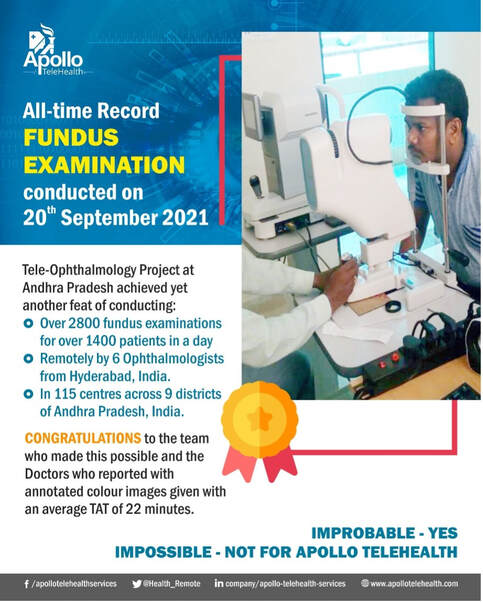
International Organization for Standardization (ISO) – An OVERVIEW The, International Standards Organization, TC 215 Health Informatics Committee developed a Technical Specification, ISO/TS 13131 Telehealth services, based on a risk and quality management approach. This standard supports healthcare planning, service and workforce planning, organization responsibilities, financial and IT management. ISO was established in 1947 in Geneva, Switzerland. An Independent, non-governmental international organization it develops standards that are recognized and respected globally. It brings experts together to improve quality and provide world-class healthcare services. Experts are from 166 national standard bodies. ISO standards are developed by various advisory groups. Presently ISO has 255 technical committees, 515 subcommittees, and 2498 working bodies. Since 1947, ISO’s technical experts have created more than 18,800 standards for all possible business. ISO standards ensure that administration and product/workflow systems are carried out legally, safely and effectively. ISO technical experts have developed several assessment protocols to ensure that certified organizations apply these guidelines in their workplace. The approved protocols aid organisations to ensure that their frameworks, devices and workforce are actually in compliance with ISO standards. ISO 13131 provides recommendations on guidelines for Telehealth services deploying Information and Communication Technology (ICT) to deliver quality healthcare services. Prof. Krishnan GanapathyDistinguished Professor at Tamilnadu Dr MGR Medical University, India & a WHO Digital Health Expert. Past President of the Telemedicine Society of India, Neurological Society of India, and Indian Society for Stereotactic & Functional Neurosurgery. Member of the Board of Directors of Apollo Telemedicine Networking Foundation and Apollo Telehealth Services, and InnovaSpace Advisory Board member - Visit: drkganapathy.com Distance is Meaningless and Geography has become History - paraphrasing Star Trek's Captain Kirk, played by William Shatner (who just flew on a sub-orbital flight on 12th October 2021 at the age of 90 years) and going where No man has ever gone before is not the prerogative of the elite 600 plus astronauts who have left the confines of Terra Firma. In an activity that would have seemed like science fiction just a few years ago, 30 Retinal Specialists have been peering into 2800 eyes a day from a distance of 175 to 350 km, and ensuring that a digitally-signed colour-coded annotated fundus report (assisted with semi-automated diagnosis) is physically provided to each villager within 25 minutes. And this has now been happening daily for the last 43 months, in a service that the beneficiary gets totally free, thanks to a Public-Private Partnership project. An acute shortage of eye care personnel in rural India results in millions unnecessarily developing visual impairment. Early diagnosis and initiation of corrective measures remotely could be a major public health initiative, whereby the Government fills a large void by providing free, quality eye care services, including spectacles, to the community. The Andhra Pradesh Government has now been implementing the “Mukhyamantri e-Eye Kendram-MeEK (http://enethraap.phc.ind.in/) program since 1st February 2018. This tele-ophthalmology service is one of the largest Public-Private Partnership projects. In just 43 months 1.7 million patients have had their eyes checked in 115 Eye centres located in 9 districts of Andhra Pradesh, a state in southern India. A total of 1.4 million spectacles have been ordered following 1.7 million refraction checks! The operational challenges in providing “customer delight” to 2000 + people every day in so many rural centres is indeed a humongous task. Some 0.5 million fundus examinations have been performed remotely and abnormal pathology detected in 83,000 cases, including Diabetic Retinopathy, Hypertensive Retinopathy, Glaucoma and other pathologies. Continuous quality control and ensuring constant compliance and adherence to strict deliverables is in the DNA of the entire fantabulous team who continued to work even during the height of the pandemic. Obsession with perfection - where failure is not an option, making the impossible possible - these are the stuff of which astronauts and the entire extended team remotely connected with space exploration are made up of. Who knows, perhaps this project is a good recruiting ground for ISRO, ESA and NASA – after all there are a lot of similarities !!
Prof. K. Ganapathy MCh (Neurosurgery), FACS, FICS, FAMS, PhDDirector Apollo Telemedicine Networking Foundation; Director, Apollo Tele Health Services; Past President, Telemedicine Society of India; Past President, Indian Society for Stereotactic & Functional Neurosurgery; Former Secretary/Past President Neurological Society of India;  I wish to thank Dr Thais Russomano for sharing with the InnovaSpace readers my article on “ Technology in Telehealth”, published in the IEEE Computer Society Region 10 newsletter. Also acknowledged is permission given by H.R. Mohan, Editor & Portfolio Member, IEEE Computer Society. The original article was for Telehealth on Terra firma ! How relevant is providing TLC ( Tender Loving Care) when the patient is 600 km above the earth and, perhaps in the future, several hundred million kms away? With failure not being an option in such an environment, both the beneficiary and the health care provider are perhaps only interested in technology per se and rightly so. Is there still a place for virtually empathising and sympathising with a patient, far away from Earth? Should we compound the already complicated milieu by taking into account the extra terrestrial patient’s wants and desires? And should the family also be involved in the decision making process or should we just leave it to an AI enabled algorithm which gives more weightage to the Microgravity environment and takes into account the lack of precedents? A media release said it all “NASA to send humans to the moon once again, – but this time we will stay“. This will also be a forerunner to the manned mission to Mars. With over 600 individuals already having gone into space in the last 55 years and space tourism having just started, extra terrestrial healthcare is now a reality. Bringing Space, down to Earth is not a pun. Representing almost 1% of global economic activity, the multiplier effect and stimulus to health and economic growth is real. There is considerable similarity between probing the emptiness of Space on distant galaxies and getting into millimetre sized capillaries in the heart and brain of the unborn – to go “ where no Man has ever gone before”. Belonging to the BC ( Before Computers - I was the last group of neurosurgeons trained in India when computers were almost non existent in a hospital ! BC is not Before Covid) era, I am Jurassic Park material and old fashioned enough to hope the super sophisticated Flight Surgeon on Earth instructing the on-board robot what to do, would still spare a few minutes and discuss with the family on Earth, the options and its limitations and advantages. Of course, we're not sure yet whether an individual space tourist / astronaut could give an Advanced Medical Directive before he leaves the Earth on a customised Informed Consent form. These ethical issues can no longer be postponed. The future is ahead of schedule. The future is yesterday not tomorrow!
Learning from terrestrial healthcare: 3 ways to get medical autonomy for deep space travel13/5/2021
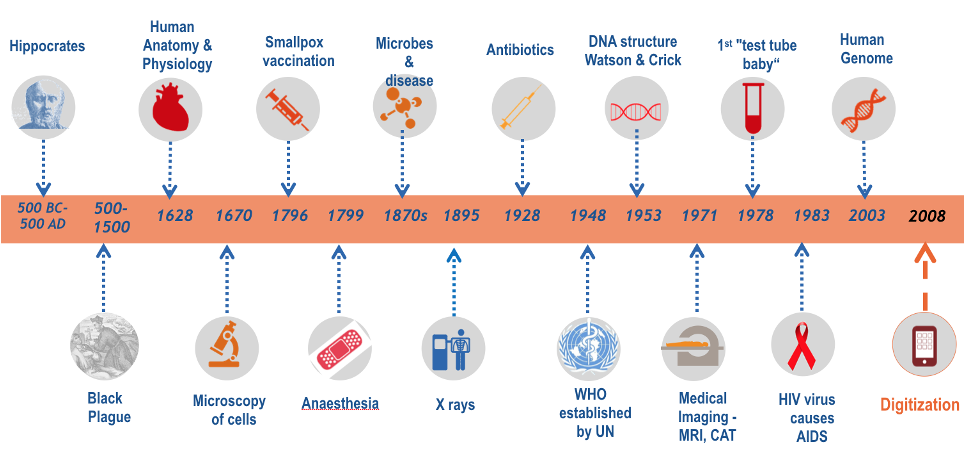
Jules LanceeBiomedical engineer, with a focus on emerging technologies and their role in the changing world of healthcare. He explores how they will impact the care delivered to patients, but is also equally interested in how they could benefit the future of long-term spaceflight. He believes both questions are opportunities for collaboration and inspiration!  SpaceX Starship landing SpaceX Starship landing How would you deal with physical and mental health needs on a three-year round-trip to Mars? Those are questions I often think about and I would like to take you on a tour of solutions already out here on Earth, that might benefit those first astronauts to the Red Planet. Last week SpaceX performed another successful test of its Starship. The Starship is designed to eventually bring as many as a 100 people to Mars per flight. We’ve seen many recent plans for human spaceflight, both commercial and non-commercial and it’s about right to say that humankind will go on more and longer duration space missions. A lot of engineering research is going into the development of rockets and other technological advancement, but just as important as getting there, will be getting there alive and healthy! That’s not a trivial problem: Especially when we will go on deep space missions to Mars and beyond we will run into some basic limitations. There will be communication delays, we will have limited medical equipment on board due to limitations in mass, volume and electricity, and limited medical skills. A doctor can come along, but the doctor can also become sick, and of course, emergency evacuation to Earth will no longer be an option. Therefore, we will need a sense of medical autonomy for those astronauts on the go. We will send the most healthy human beings on such a mission, but a 3-year trip is a long time to stay healthy in the extreme environment of outer space. If not physical problems, then also psychological issues can become a risk to the success of the mission, which the crew themselves will need to deal with. In this quest for medical autonomy, I argue, we can learn from trends in healthcare and healthcare innovation on Earth, so let’s shortly take a trip back to Earth. In this short overview of the history of healthcare, a lot has happened since Hippocrates worked out the oath for medical professionals. None of the developments shown however, were as fundamental as the last one, the advent of digital health technologies. By becoming digital, solutions for healthcare have become smaller, faster, cheaper and in many cases, smarter. Solutions are leveraging Artificial Intelligence, Virtual and Augmented Reality, blockchain, voice recognition and 3D printing. These are just some of the technologies that are impacting healthcare.
As a result of this impact, we see various shifts in healthcare, going from a reactive system to more preventive care and from a one-size-fits-all-healthcare to precision medicine. Most importantly, however, you see a shift in power. The relationship between the doctor and his or her patient is changing from a more dependent relationship, into a partnership, in which the patient is empowered with technology, to take care of his/her own health or medical issues. In other words, terrestrial patients are becoming more autonomous when it comes down to their health and care. It is this change, that is also needed for astronauts on their way to Mars. A different relationship between astronauts and their doctors in mission control is needed and this can be achieved, by leveraging new health technologies. Here are 3 terrestrial examples:
We welcome another blog by ESA-sponsored Dr Stijn Thoolen, currently spending 12 months at the Concordia research station in Antarctica conducting experiments. What an amazing experience - do take a look at his previous blogs (Part 1, Part 2, Part 3) to follow his great adventure to the world's southernmost continent.
Dr Stijn ThoolenMedical Research Doctor, Concordia Research Station, Antarctica
Concordia, February 7, 2020
Sunlight: 24 hours (but not for long) Windchill temperature: -45°C Mood: a little roller coaster At this moment I am just plain excited. Next to me the rest of the DC16 crew are having their own emotions. Our freshly inaugurated station leader Alberto, draped in the colours of our three national flags, came up with the idea to have our national anthems playing while the last Basler plane of the summer campaign leaves Dome C. So here I stand, hearing my own voice on maximum volume pronouncing a Dutch translation of too patriotic sentences from the station’s speakers, and with the Dutch ‘Wilhelmus’ screaming over the Antarctic plateau as an official start of our winter over. Haha, such an unrealistic scenario! And while those sounds are quickly overruled by the roaring engines of the plane, and with snow blowing in our faces, I can only smile. There goes our last connection to the rest of the earth, disappearing into the distant sky. Unbelievable!
I guess I have already spilled all of my emotions at this point. In the past few days, more and more planes have been taking away more and more of the beautiful people we enjoyed our summertime with, and the station has become more and more empty. Funny: they were already leaving, and I have the idea we just started… It has been an exciting idea on the one hand, but the closer we came to being left alone, the more and more confronting that got on the other. When two days earlier another plane left with sixteen more people, the goodbyes were harsh, with everyone in tears again. You know, those healthy ones. And when it was gone, those left on the ice slowly returned back to the station, all silent, all caught in their own thoughts. It had been an intense few summer months, and this was the weird moment of realization that it had come to an end, with a big unknown lying ahead. I guess the blend of feelings has been a repetition of those during the days before my departure to the Antarctic. Perhaps a little lighter this time.
Daniel E. Vigo, MD, PhD Independent Researcher: Institute for Biomedical Research (Catholic University of Argentina and National Scientific and Technical Research Council) & InnovaSpace Advisory Board Member Belgrano to MarsThe Antarctic continent is considered to be one of the most realistic analogues found on Earth of the situations of extreme isolation and confinement experienced in space. Since 2014, we have been conducting at the Belgrano II Argentine Antarctic Station the project "Chronobiology of Antarctic Isolation: the use of the Belgrano II Station as a model of biological desynchronization and spatial analogue", also known as “Belgrano to Mars”. The project aims to explore the impact of a year of isolation on different physiological, psychological and social variables. In particular, we are interested in studying how biological rhythms are affected by the lack of natural light during the four months of polar night typical of that latitude. The study of the chronobiological responses to extreme isolation increases our understanding of the physiological mechanisms underlying human biological rhythms, with applications in space exploration or other highly demanding professional settings, as well as in human health. The Belgrano II Antarctic station consists of a series of scientific research facilities located approximately 1,300 km away from the South Pole at 34°S, 77°W. It is the most southerly Argentinian station and one of the three southernmost permanent stations on the planet. The temperature ranges from 5°C to 48°C below zero. One feature of this station is that, due to its latitude, it has four months of continuous sunlight, four months of twilight and four months of polar night. The station crew is composed of around 20 men. To generate a light-dark cycle during the summer, windows with blinds closed are used, in accordance with a normal sleep routine, while using eye covers during the night if necessary. Exposure to ultraviolet light is also stronger and sunglasses for external work are mandatory. Conversely, in the wintertime, the light-dark cycle depends entirely on artificial light. Schedules with well-defined times for meals (breakfast, lunch and dinner) work and rest are paramount in Antarctic stations. “Belgrano to Mars” is a collaborative project in which researchers Camila Tortello and Santiago Plano (UCA-CONICET and UNQ) participate in the analysis and interpretation of the information and Juan Manuel Cuiuli (Joint Antarctic Command) in the scientific coordination between Buenos Aires and Antarctica. Other members of the project are Marta Barbarito (Argentine Antarctic Institute), Diego Golombek and Patricia Agostino (UNQ and CONICET), Agustín Folgueira and Juan Manuel López (Central Military Hospital), and Guido Simonelli (University of Montreal). Field work during isolation is carried out by physicians from the wintering crews at the station and staff members that volunteer for the study. Antarctic scientific activity is coordinated by the National Antarctic Directorate (DNA), which together with the Joint Antarctic Command, provides the logistics of the bases. TelemedicineThis year, we have traveled to Antarctica to supervise the implementation of the Belgrano to Mars project in the field, to test measurement instruments and to train the crew in the use of the equipment and software. The trip demanded six weeks of navigation in the ARA Almirante Iríza icebreaker. In addition, we started working with the European Space Agency (ESA) in the operational test of the Telemedecine Tempus Pro equipment, under the framework of an ESA-CONAE-DNA agreement. The project, led by Dr. Víctor Demaría-Pesce, from ESA's European Astronaut Center, involves conducting operational simulations in a situation of extreme isolation and confinement, which will contribute to the design of a definitive prototype to be used by astronauts and medical teams during future space missions to the Moon and Mars. The equipment will be tested at Belgrano II (Dr. Bruno Cauda and Enf. Luis Almaraz) and Carlini (Dra. Melina D'Angelo and Enf. Gustavo Cruz) stations, through six simulations that will recreate medical scenarios similar to those encountered by astronauts in space. Lessons to be learned from this kind of study We have recently published in the journal Scientific Reports (from the Nature Group) data regarding changes in the sleep-wake cycle during a winter campaign at Belgrano II. We observed that during the polar night the subjects tended to go to bed one hour later and sleep one hour less. A possible explanation is that this is due to the lack of exposure to natural light, since bright light acts as a synchronizer of our biological rhythms. This loss of sleep was somewhat compensated by naps, which were longer during that time of year.
These results show us how biological rhythms can be desynchronized in periods of prolonged confinement, such as the ones we have had to go through during the quarantine periods instituted in different countries. Moreover, it highlights the importance of exposure to natural light in the morning and darkness during the night and maintaining fixed activity and rest routines to avoid the desynchronization of our biological rhythms. Other sleep hygiene measures include the limiting of daytime naps to 30 minutes, regularly exercising (it may be necessary to avoid working out before bedtime), having a light dinner, avoiding stimulants like caffeine and nicotine close to bedtime, and making sure that the sleep environment is dark, silent and with a pleasant temperature. The beneficial effects of having good sleep relate to an increase in alertness during the day, the prevention of anxiety or depression, and the improvement of our general health, which in turn will reduce the chances of becoming ill. Author: Nina Louise PurvisMedical student, Queen Mary University of London; Postgraduate Researcher, King’s College London 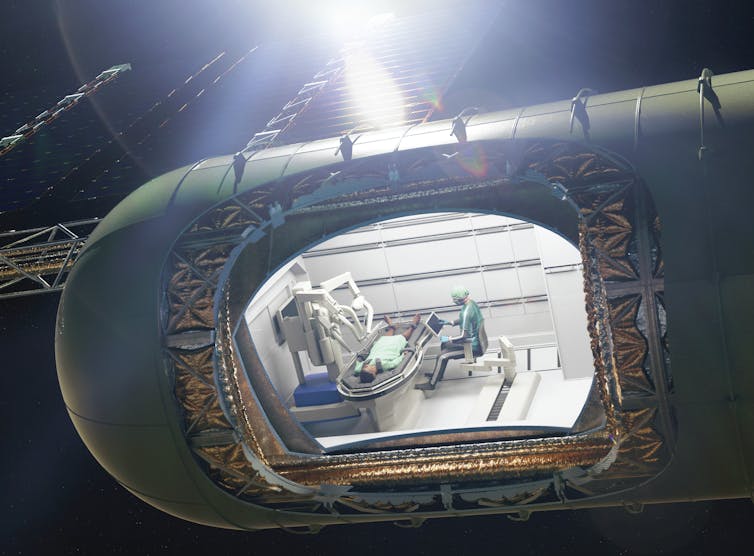
Earlier this year, it was reported that an astronaut in space had developed a potentially life-threatening blood clot in the neck. This was successfully treated with medication by doctors on Earth, avoiding surgery. But given that space agencies and private spaceflight companies have committed to landing humans on Mars in the coming decades, we may not be so lucky next time. Surgical emergencies are in fact one of the main challenges when it comes to human space travel. But over the last few years, space medicine researchers have come up with a number of ideas that could help, from surgical robots to 3D printers. Mars is a whopping 54.6 million kilometres (33.9 million miles) away from Earth, when closest. In comparison, the International Space Agency (ISS) orbits just 400 kilometres above Earth. For surgical emergencies on the ISS, the procedure is to stabilise the patient and transport them back to Earth, aided by telecommunication in real time. This won’t work on Mars missions, where evacuation would take months or years, and there may be a latency in communications of over twenty minutes. As well as distance, the extreme environment faced during transit to and on Mars includes microgravity, high radiation levels and an enclosed pressurised cabin or suit. This is tough on astronauts’ bodies and takes time getting used to. We already know that space travel changes astronauts’ cells, blood pressure regulation and heart performance. It also affects the body’s fluid distribution and weakens its bones and muscles. Space travellers may also more easily develop infections. So in terms of fitness for surgery, an injured or unwell astronaut will be already at a physiological disadvantage. 
But how likely is it that an astronaut will actually need surgery? For a crew of seven people, researchers estimate that there will be an average of one surgical emergency every 2.4 years during a Mars mission. The main causes include injury, appendicitis, gallbladder inflammation or cancer. Astronauts are screened extensively when they are selected, but surgical emergencies can occur in healthy people and may be exacerbated in the extreme environment of space. Floating intestinesSurgery in microgravity is possible and has already been been carried out, albeit not on humans yet. For example, astronauts have managed to repair rat tails and perform laparoscopy – a minimally invasive surgical procedure used to examine and repair the organs inside the abdomen – on animals, while in microgravity. These surgeries have led to new innovations and improvements such as magnetising surgical tools so they stick to the table, and restraining the “surgeonaut” too. One problem was that, during open surgery, the intestines would float around, obscuring view of the surgical field. To deal with this, space travellers should opt for minimally invasive surgical techniques, such as keyhole surgery, ideally occurring within patients’ internal cavities through small incisions using a camera and instruments. A laparoscopy was recently carried out on fake abdomens during a parabolic “zero gravity” flight, with surgeons successfully stemming traumatic bleeding. But they warned that it would be psychologically hard to carry out such a procedure on a crew mate. Bodily fluids will also behave differently in space and on Mars. The blood in our veins may stick to instruments because of surface tension. Floating droplets may also form streams that could restrict the surgeon’s view, which is not ideal. The circulating air of an enclosed cabin may also be an infection risk. Surgical bubbles and blood-repelling surgical tools could be the solution. Researchers have already developed and tested various surgical enclosures in microgravity environments. For example, NASA evaluated a closed system comprising a surgical clear plastic overhead canopy with arm ports, aiming to prevent contamination. When orbiting or settled on Mars, however, we would ideally need a hypothetical “traumapod”, with radiation shielding, surgical robots, advanced life support and restraints. This would be a dedicated module with filtered air supply and a computer to aid in diagnosis and treatment. Robots and 3D printingThe surgeries carried out in space so far have revealed that a large amount of support equipment is essential. This is a luxury the crew may not have on a virgin voyage to Mars. You cannot take much equipment on a rocket. It has therefore been suggested that a 3D printer could use materials from Mars itself to develop surgical tools. Tools that have been 3D printed have been successfully tested by crew with no prior surgical experience, performing a task similar to surgery simply by cutting and suturing materials (rather than a body). There was no substantial difference in time to completion with 3D printed instruments such as towel clamps, scalpel handles and toothed forceps. 
Robotic surgery is another option that has been used routinely on Earth, and tested for planetary excursions. During NEEMO 7, a series of missions in the underwater habitat Aquarius in Florida Keys by NASA, surgery by a robot controlled from another lab was successfully used to remove a fake gallbladder and kidney stone from a fake body. However, the lag in communications in space will make remote control a problem. Ideally, surgical robots would need to be autonomous. There is a wealth of research and preparation for the possible event of a surgical emergency during a Mars mission, but there are many unknowns, especially when it comes to diagnostics and anaesthesia. Ultimately, prevention is better than surgery. So selecting healthy crew and developing the engineering solutions needed to protect them will be crucial. This article is republished from The Conversation under a Creative Commons license. Read the original article. |
Welcometo the InnovaSpace Knowledge Station Categories
All
|
||||||||||
UK Office: 88 Tideslea Path, London, SE280LZ
Privacy Policy I Terms & Conditions
© 2024 InnovaSpace, All Rights Reserved












 RSS Feed
RSS Feed