Author: Dr. Paul ZilbermanMedical Doctor, Anaesthetist, Hadassah Medical Center Jerusalem, Israel
Space is very different, in many aspects. This post does not attempt to address the many changes the human body experiences in space, such as volume modifications in body compartments, fluid shifts, structural configuration in receptor* morphology and, as a consequence, possible variations in pharmacology response, etc. * For the lay reader, a receptor is a special structure on the surface of a cell, for example, that functions as a "receiving point" on which a chemical substance acts in a unique way (like a key – lock mechanism) and a specific reaction is generated (like a muscle contraction) or inhibited (like a cork closing a bottle and blocking the passage of a fluid). These complex structural changes modify many biological reactions, as well as the body’s response to medications. Rather, this post presents some of the technical challenges that an anaesthesiologist may encounter in space. Confined space. On Earth gravity keeps everyone’s feet on the ground. Different pieces of equipment can be repositioned depending on the procedure, machinery can be brought in as needed (XRay scans in orthopaedics, for instance), electric cables can be switched to other convenient wall sockets etc. In a fixed volume space capsule, you don’t have all these possibilities. Everything is measured for maximum volume efficiency. Taking into consideration that anything can and will float if not properly anchored, we can imagine what an “anaesthesia dance” could happen! What equipment? On Earth an anaesthesia workstation is always present in the OR. Depending on its complexity its volume can vary between a medium size fridge to a large double-doored one, just put on its side. You don’t have this amount of deposit in a space cabin, but let’s suppose for one moment that you do - you then need an Anaesthesia Gas Scavenging System (AGSS), which removes the anaesthesia gases that have leaked out or at the end of the procedure. On Earth, these gases are expelled into the atmosphere (there is a lot to talk about this and the greenhouse effects too) and the air currents around any medical facility carry them away. In space you don’t have this. Any gas must be expelled using energy, an active process. Otherwise, the whole cabin will become a big anaesthesia machine with all crew members affected. And, speaking of energy, an anaesthesia workstation is also powered by electricity, which is a limited resource in space, depending on the surface of the solar (or light in general) panels. This energy must be stored and used for other life maintenance systems as well, of which a critical example is the Sabatier reactor that provides oxygen. Regional anaesthesia The simplicity and portability of the necessary equipment makes this type of anesthesia attractive. For peripheral neural blocks all you need is a simple ultrasound machine and dedicated needles. The potential drawbacks are that the technique/s need to be taught on Earth but their “transposition” to space is a bit problematic. If the spinal/epidural anaesthesia is relatively simple to learn, the USG (ultrasound guided) blocks are more challenging. Furthermore, the bodily fluid shift due to the lack of gravity causes many tissues to change their tridimensional appearance, leading to increased difficulty in performing the block.
The cardiovascular responses that accompany spinal/epidural anaesthesia on Earth, in terms of heart rate and blood pressure, are different in space. There may be a lack of reactivity so a certain reduction in blood pressure, for example, might not be compensated. We need to remember that the hostile environment in space, especially radiation, affects not only the human body, but also many sensitive electronic components of medical equipment, leading to possible dysfunction. Monitors can potentially de-calibrate and all the information you receive may become inaccurate. Fluids Preparing and administering a fluid on Earth is routine, however, the lack of gravitation in space poses other challenges: air and fluids do not mix. It is called “lack of buoyancy”. Unless we use special equipment to separate fluids from air nothing can be delivered to the patient. This statement is true also for the anaesthesia vaporiser (a special closed recipient that contains the anaesthesia substance); not only can you not simply fill it the way it would be done on Earth, but even if you could, the anaesthesia liquid that becomes vapour cannot separate from the fluid from which it originates. It just cannot exit the vaporiser. Below is a small example of how liquids behave in space and what happens when a liquid exits a recipient: The same is true for another type of anaesthesia, called TIVA = Total Intra Venous Anaesthesia. This technique uses a dedicated syringe pump that pushes different anaesthesia substances through an intra venous line. It’s a useful technique both in terms of volume and energy expenditure, but again we face the same problems: how to fill the syringe without air bubbles and how to protect the electronics of the syringe pump (in fact a computer in all respects) from the deleterious influences of space radiation!
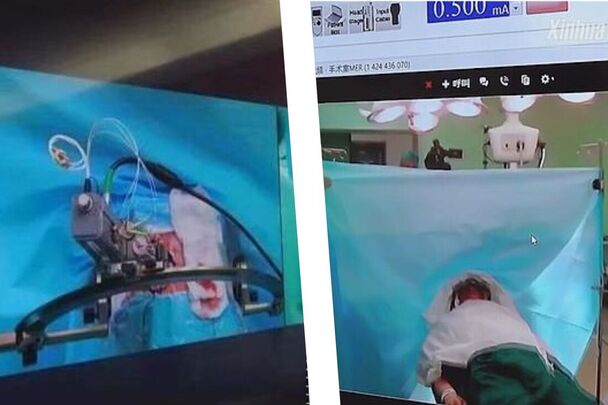
As you can see, space medicine is a very important topic and many people dream of its future use. Yet, we still have a long way to go! With the advent of intermediary space “stops” and the continuous development of new technologies, every challenge will be solved, sooner or later. Author: Prof K GanapathyDirector Apollo Telemedicine Networking Foundation, Apollo Tele Health Services | Distinguished Visiting Professor IIT Kanpur | Distinguished Professor The Tamilnadu Dr MGR Medical University | Emeritus Professor National Academy of Medical Sciences  5G is the fifth generation of wireless communication technology, promising faster data transfer speeds, lower latency (round trip latency >10 milliseconds), increased network capacity (1 million devices per sq km), 99.999% network reliability and battery life of up to 10 years for IoT devices. There is considerable hype in the media that deployment of 5G will revolutionize healthcare by enabling new medical applications and improving existing ones. Using Edge computing, 5G Data can be processed closer to where it is generated. IoMT (Internet of Medical Things) devices generate huge amounts of data. Cloud computing can provide the necessary infrastructure to process and analyze this data. Faster transmission of data will enable more efficient storage in the cloud. Accessing more bandwidth and computing resources, and providing infrastructure to enable scalability will now be less problematic. No doubt clarity of images transmitted will be better and the immersive experience in video conferencing will be an all-time high. Mammograms, CT, MRI, and ultrasound images generate large amounts of data. High-speed transfer and processing will save a few minutes. Onboard cameras, camera-based Headgear, and ‘Body Cams’ for paramedics can transmit patient data to hospitals in real-time using ultra-fast and low-latency 5G connected ambulances, with medical equipment, patient monitoring applications and telemetry devices that ensure excellent pre-hospital management. 5G can facilitate real-time control of medical robots, enabling precise and safe interventions in performing complex procedures. 5G enables faster and more efficient data transfer, facilitating clinical trials and drug development, as these require the collection of large amounts of data from multiple sources.
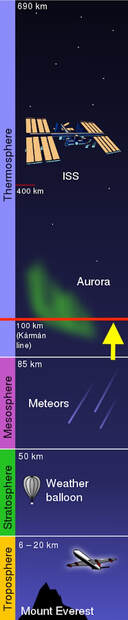
Author: Dr. Paul ZilbermanMedical Doctor, Anaesthetist, Hadassah Medical Center Jerusalem, Israel This article addresses the notion of buoyancy and why drinking beer in space (the ISS usually orbits in the thermosphere), or any carbonated drink for that matter, does not produce the known tingling sensation we can feel in our noses here on Earth. So let’s first briefly consider what is buoyancy? In simple terms, whenever an object is put into a fluid there are several forces that act upon it. The liquid exerts a force from the bottom upwards that tries to push that object up. Then there is the liquid force itself, let’s call it weight, that pushes an object downwards. However, because the liquid pressure increases the deeper you go down into the fluid, there will always be an upwards force bigger than the downward force. This can be explained by looking at the formula for hydrostatic pressure: Hydrostatic pressure = pgh In this formula, p is the density of the liquid, g is the gravitational force (9.81 m/s2) and h is the height of the fluid column measured from the surface. Keeping all the other parameters of the formula constant, the "h" at the bottom of a submerged object will be higher than the one at its top. But we also have here another component: the "g". Well, there is practically no "g" in space, unless we artificially produce it. So, in this case, all the objects inserted or included into a fluid will just stay there. Of course, there are many other factors that play a role here, for example the superficial tension of the fluids etc., however, for the sake of simplicity I am considering here only the buoyancy. So, nothing happens with the CO2 bubbles inside the fluid because they are no lighter than the fluid that surrounds them, perhaps looking something like in this photo: This not mixing between the fluid and gases within creates a hard enough life for anyone who would like to enjoy a beer in space (hypothetically, at least as alcohol consumption is not permitted on the ISS), but let's also not forget the cabin temperature of roughly 20 degrees Celsius, which is way too high to enjoy an ice cold beer. If you want to cool it a bit forget leaving it outside too - just take a look at what the temperatures are "outside", unless of course you want to lick your beer like an ice-cream!
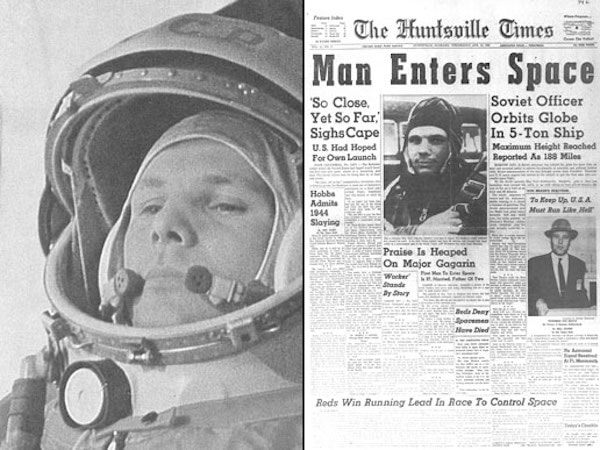
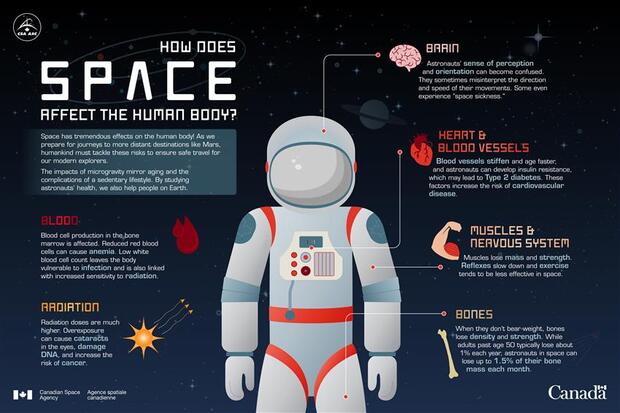
Author: Lucas RehnbergNHS Doctor - Anaesthetics & Intensive Care | MSc Space Physiology & Health  My name is Lucas, I am a doctor in the UK working in anaesthetics (or Anaesthesiology for any American readers) and intensive care medicine. I have had an interest in space medicine for over 10 years now, inspired by none other than Prof Thais Russomano who has mentored me over the years and still does. My Master’s dissertation (back in 2009) focused on CPR (cardiopulmonary resuscitation) methods in microgravity, with my continued research interest surrounding critical care in space. I am careful to say that I am a doctor with an interest in space medicine and physiology, as opposed to a ‘Space Doctor’ – as there are many individuals out there who have committed many more years than I have to this field and are vastly more experienced than I am! A club I aspire to join one day. The idea of this blog, or series of blogs, is to look at some of the latest research in space physiology and space medicine, then consider how this will play out clinically. With a particular focus on critical care and potentially worst-case scenarios when in space (or microgravity environment). Something all doctors will have done in their careers; we are equipped with the skills to critically appraise papers and then ask if they are clinically relevant, or how will it change current practice. Over the last 60 (ish) years of human space flight, there is lots of evidence to show that there are many risks when the human body has prolonged exposure to microgravity, which can affect most body systems – eyes, brain, neuro-vestibular, psychological, heart, muscle, bone, kidneys, immune system, vasculature, clotting and even some that we haven’t fully figured out yet. But then what needs to be done is to tease out how clinically relevant are these from the research, how could that potentially play out if you were the doctor in space, then how to mitigate that risk and potentially treat it.
Author: Tobias Leach3rd Year Medical Student | University of Bristol | Passionate about space! Space provides boundless opportunities for human existence and innumerable threats to human health. The question is, are we yet prepared to deal with a catastrophic event, such as a cardiac arrest in space? Abstract
Introduction To gain an understanding of the current state of CPR in microgravity with a focus on chest compressions in the event of a sudden cardiac arrest onboard. Methods An Ovid Medline search was conducted: 17 articles were found; 12 were excluded; six additional articles were found in the references of the remaining five articles, bringing the total number of articles included to 11. These were then critically analysed. Results No CPR method currently reaches the European Resuscitation Council (ERC) guidelines. The Handstand (HS) method appears to be the strongest. Evetts-Russomano (ER) is the second strongest method. Automatic chest compression device (ACCD) performed consistently well. Conclusion CPR appears to be far more difficult in microgravity. Inconsistencies in research methodology do not help. The ER method should be used as a first contact method and the HS method should be used once the casualty is restrained. An ACCD should be considered as part of the medical equipment. Further research is needed, directly comparing all positions under the same conditions. Author: Prof. K. GanapathyHon Distinguished Professor The Tamilnadu Dr MGR Medical University; Emeritus Professor, National Academy of Medical Sciences; Past President, Telemedicine Society of India & Neurological Society of India; Director Apollo Telemedicine Networking Foundation & Apollo Tele Health Services, India ABSTRACT: Introduction: Metaverse is the augmented virtual world formed by convergence of virtual and physical space. Users interact within this created world, meeting each other virtually, immersing themselves in performing virtual activities, which subsequently could lead to real experiences. Conventionally, the healthcare “industry” is conservative in deploying future ready technology. Aims and Objectives: This overview discusses the untapped potential of metaverse applications in healthcare from a clinician’s perspective. Bereft of technical jargon, the article points out the advantages, disadvantages, limitations, and challenges in actual deployment of the metaverse in clinical practice in the real world. The exponential transformation occurring in this area is highlighted. The highly technical literature is simplified for easier comprehension. Findings: Clinical applications, use of the metaverse in training, education, and augmenting telehealth consultations, in an immersive milieu, is discussed. Direct “in-person” interaction with digital products and solutions will be a new experience for a healthcare provider and the beneficiary. The role of digital twins is illustrated. Consultation process and various clinical applications in the metaverse are outlined. Technology‑enabled futuristic training and education is discussed. Conclusion: Demonstrating significant improvement in healthcare outcomes using the metaverse will be difficult to prove. This alone will ultimately lead to the development of a business model, insurance reimbursement and behavioral modification necessary for accepting and using, a hitherto unused method in patient care. Keywords: Augmented reality and healthcare, blockchain and healthcare, metaverse and healthcare, virtual reality and healthcare The full article can be read and freely downloaded following this LINK
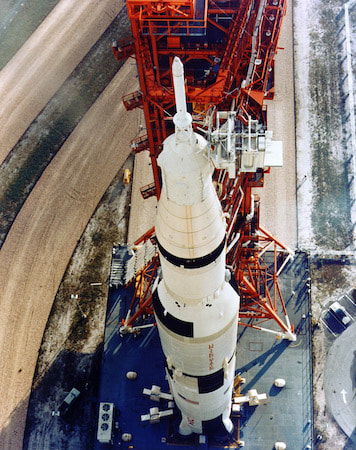
Author: Paul Zilberman MDAnaesthesiologist, Israel MOTTO: I was born in 1960. As a child I was thrilled to witness the first man in space, as per stories, in those years a direct TV transmission was still a dream. And even if it had been possible, I was one year of age, so… But later on, I was able to see the launch of the Apollo missions and the common US-Soviet programs Soyuz- Apollo. As many other terrestrials I was thrilled to watch, both from distance and close up, those “white pencils” with the painting of “The United States of America” climbing faster and faster, leaving behind a huge ball of fire… Then the first carrying rocket segment detaching and falling back to Earth… I was amazed seeing how only after a short time those “people out there” were floating and smiling, waving their hands and telling us everything is ok. I was reading about the many experiments that were carried out during the flights, I was even able to look now and then at the flight path, little understanding what were the sinusoidal lines appearing on the huge Command Center screen, where so many people were sitting in front of the computers with the microphones and earpieces connected. I didn’t understand then, exactly, why so many people were dealing with so few in space.
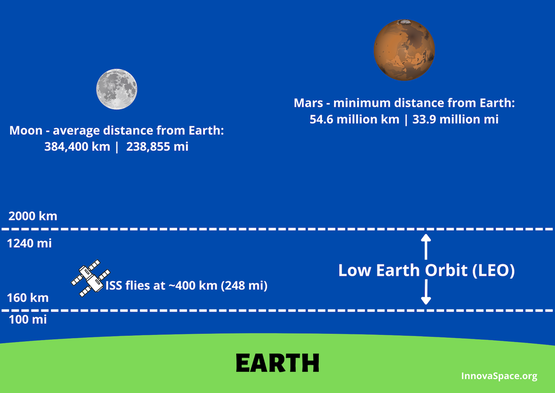
Well, time went on, Skylab appeared, then the ISS, the shuttles…wow…all in a lifetime. As time went on and understanding grew, on top of my medical school and, later on, anaesthesia residency, other questions arose: how do the astronauts eat, drink, wash, use the toilets? And many other daily mundane things we take for granted down here. Author: Rohan KrishnanUndergraduate, Bachelor of Science - Statistics & Healthcare Management | The Wharton School, University of Pennsylvania In 1955, Walt Disney’s “Mars and Beyond” pondered human survival in extraterrestrial environments. The narrator envisions the colonisation of Mars as a feasible reality: a future where cities are encased in pressurised domes on the Red Planet to combat overpopulation and the depletion of natural resources on Earth. Today, NASA’s Artemis Mission plans to return astronauts to the moon by 2025, this time with an eye toward lunar colonization and human exploration of Mars. The boundaries that once constrained human space exploration are shattering, as technological advancements and ambitious government space programs bring plans for travel to Mars closer to reality. Beyond government space agencies, private companies like Blue Origin and SpaceX are innovating to create faster, more efficient aircraft and bring space travel to the masses through commercial flights. As astronauts inch toward deep space missions, understanding the general health risks of long-distance space travel, as well as the varied conditions between environments, is crucial. Missions to the International Space Station (ISS) and in low Earth orbit (LEO) have uncovered a variety of consequences for astronaut health, including bone loss, muscle atrophy, and a weakened immune system, amongst others. Radiation, microgravity, the distance from Earth, isolation, and the hostile environment inside spacecraft are the root causes behind the health issues that astronauts experience in space. Space exploration is vital for advancing life on Earth. Future missions across our solar system can help us understand the effects of microgravity and radiation on biological systems, locate valuable natural resources, and even combat overpopulation by exploring space colonisation. Given this need, ensuring the health of humans in space is the bedrock for further discovery. In this blog, I will describe the significant health challenges associated with with spending time in LEO and on long-distance spaceflight to the Moon and Mars. I have narrowed the focus to the following branches of medicine, to outline and contrast the particular health issues between LEO and long-distance spaceflight: cardiology, ophthalmology, and neurology. Many of the health concerns associated with time spent in LEO persist during long-distance space travel, but there are also challenges specific to the Moon and Mars stemming from their unique environmental characteristics, such as the presence of regolith and varying radiation levels. Understanding these general and environment-specific health concerns will inform planning as we venture deeper into space.
<
>
The vast majority of human spaceflight has occurred within low Earth orbit (LEO), with the notable exception of the Apollo program’s lunar missions. All manned space stations, including the ISS, are in LEO. As a result, for more than two decades, countless experiments have been conducted on the ISS to understand how astronauts’ health is impacted in LEO.
CardiologyResearchers studying the health of astronauts aboard the ISS have uncovered that long-term travel in LEO has notable effects on astronauts’ cardiovascular health. According to Dr. Thais Russomano, a leading expert on space medicine, the absence of Earth’s gravitational force in space causes bodily fluids and blood to shift from the legs and lower abdomen toward the upper torso and head. This phenomenon - referred to as ‘puffy-face and bird-legs syndrome’ - causes swelling in the face and head while reducing astronauts’ circulating blood volume and heart size. As less blood is pumped by the heart in microgravity, astronauts endure muscle loss in the heart, placing them at risk for cardiovascular deconditioning and cardiac myocyte atrophy.
Radiation is another significant concern impacting astronauts’ cardiovascular health. Aboard the ISS, radiation from galactic cosmic rays, solar cosmic rays, and particles from the Van Allen radiation belts are of primary concern. Astronauts are exposed to roughly 40-times more millisieverts of radiation compared to people on Earth. Exposure to space radiation over long-term missions increases astronauts’ risk for cancer and cardiovascular diseases, although effective shielding and radiation shelters aboard spacecraft have helped mitigate those risks. Cardiovascular issues resulting from microgravity and radiation exposure over long periods aboard the ISS can follow astronauts well after returning to Earth. Some studies have determined that astronauts’ arterial blood pressure decreased throughout space missions due to the loss in circulating blood volume, although there could be many causes behind this change. Similarly, the reduction in circulating blood volume can cause orthostatic intolerance - the inability to stand due to lightheadedness or fainting - once astronauts return to Earth. Although radiation exposure and microgravity cause cardiovascular problems in space, studies on astronaut mortality have concluded that astronauts are at a lower risk of death from cardiovascular diseases relative to the general population on Earth. OphthalmologyThe effects of bodily fluid shifting in microgravity extend beyond ‘puffy-face and bird-legs syndrome’, with consequences for the eyes. Following a six-month mission to the ISS in 2005, astronaut John Phillips’s perfect vision was found to have deteriorated due to spaceflight-associated neuro-ocular syndrome (SANS). SANS is formerly known as visual impairment and intracranial pressure (VIIP) syndrome, although the name was updated to reflect the uncertainty over whether increased intracranial pressure is the sole cause of the condition. One explanation is that SANS is caused by cerebrospinal fluid shifting toward the head, increasing intracranial pressure, particularly at eye level. The pressure causes the back of the eye to flatten, resulting in a hyperopic shift and blurred vision.
According to a report from the British Journal of Anaesthesia, a questionnaire of 300 astronauts found that 28% of short-duration mission astronauts and 60% of long-duration mission astronauts experienced degradation of visual acuity. A study of seven long-duration mission ISS astronauts and nine short-duration mission space shuttle astronauts found that the long-duration astronauts had significantly greater post-flight flattening when compared with the short-duration astronauts. Given the increased severity of SANS on long-duration missions, understanding causes and possible treatments are vital for exploration in and beyond LEO. NeurologyMicrogravity has notable effects on the nervous system, particularly due to the redistribution of bodily fluids in space. Neuroimaging scans show that astronauts’ brains have increased ventricular volumes following long-distance spaceflight. As fluids shift toward the upper torso and head during long-term exposure to microgravity, the volume of cerebrospinal fluid collected in the brain’s ventricles increases, resulting in ventricular expansion. Ventricular expansion could be a possible cause of SANS and may be linked to premature ageing of the brain. One study found that astronauts who spent 12 months in space displayed larger changes in ventricular volume than astronauts who spent 6 months in space, suggesting important implications for long-duration space missions. The microgravity-induced fluid shift is also associated with alterations to white matter in astronauts’ brains. A study from the journal Science Advances reports that cosmonauts displayed increased white matter in the cerebellum following long-duration spaceflight, with white matter volume returning to roughly pre-flight levels seven months after spaceflight. The cerebellum handles fine motor control, postural balance, and oculomotor control, and white matter changes associated with spaceflight may offer evidence for motor system neuroplasticity. Various studies are employing different techniques to evaluate white matter changes due to spaceflight, which could affect other neurological functions including visual and sensory processing. The health issues associated with LEO are also relevant for long-distance space travel. However, there are also environment-specific challenges unique to the Moon and Mars - such as high levels of space radiation and varying magnitudes of microgravity - that will be of primary concern to astronauts. Various studies simulate deep space environments to predict the effects of long-distance spaceflight on human health, informing mitigation strategies to keep astronauts safe.
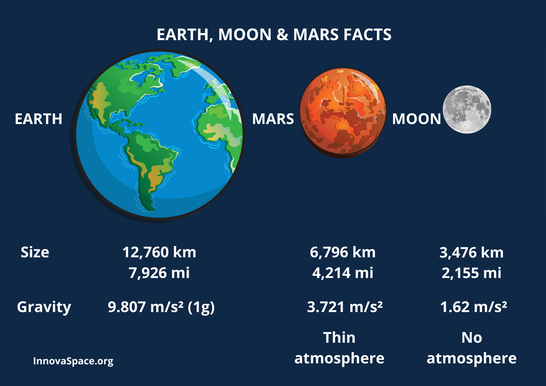
CardiologyIn deep space, the microgravity environment induces similar cardiovascular effects to what astronauts experience in LEO. Blood and bodily fluids shift toward the upper torso and head resulting in ‘puffy-face and bird-legs syndrome’, while the decreased cardiac workload can lead to cardiovascular deconditioning. However, relative to the gravitational force in LEO of approximately 0.95g, the Moon’s gravitational force is 0.16g while Mars’ gravitational force is 0.36g. It is unclear whether varied microgravity conditions will produce additional cardiovascular effects beyond those studied in LEO, however, fluid shifts and cardiovascular deconditioning remain significant concerns.
Radiation-induced cardiovascular disease is another major challenge with traveling to the Moon and Mars. Compared to missions in LEO, the space radiation environment beyond LEO exposes astronauts to higher dose rates of HZE particles, the high-energy heavy ions of galactic cosmic rays. HZE particles are highly penetrating and can cause secondary radiation when interacting with shielding in spacecraft or spacesuits. According to the journal Frontiers in Cardiovascular Medicine, high doses of HZE particles over long-term deep space missions can lead to myocardial remodelling and fibrosis, potentially resulting in heart failure. While current shielding technology may protect astronauts in LEO, the power of HZE radiation makes more advanced shielding essential to protect astronauts in deep space. OphthalmologyConsidering the microgravity-induced fluid shifts that astronauts experience in deep space, SANS remains a primary concern for missions to the Moon and Mars. SANS is typically studied on long-duration missions, although astronauts have reported blurred vision after only two weeks aboard the ISS. A mission to Mars would take up to 20 months and would require astronauts to encounter multiple gravity fields. The long duration and complex gravity shifts associated with deep space missions could cause more challenging SANS-related ocular issues compared to those faced by astronauts in LEO. The concerns surrounding radiation beyond LEO extend to ocular health. Galactic cosmic radiation has been linked to the development of phosphenes and cataracts, while studies show that repetitive spaceflights and high-radiation-dose exposure increase the prevalence of both conditions among astronauts. Considering the high volume of HZE radiation that deep space astronauts will be exposed to, the development of phosphenes and cataracts is of major concern for their ocular health.
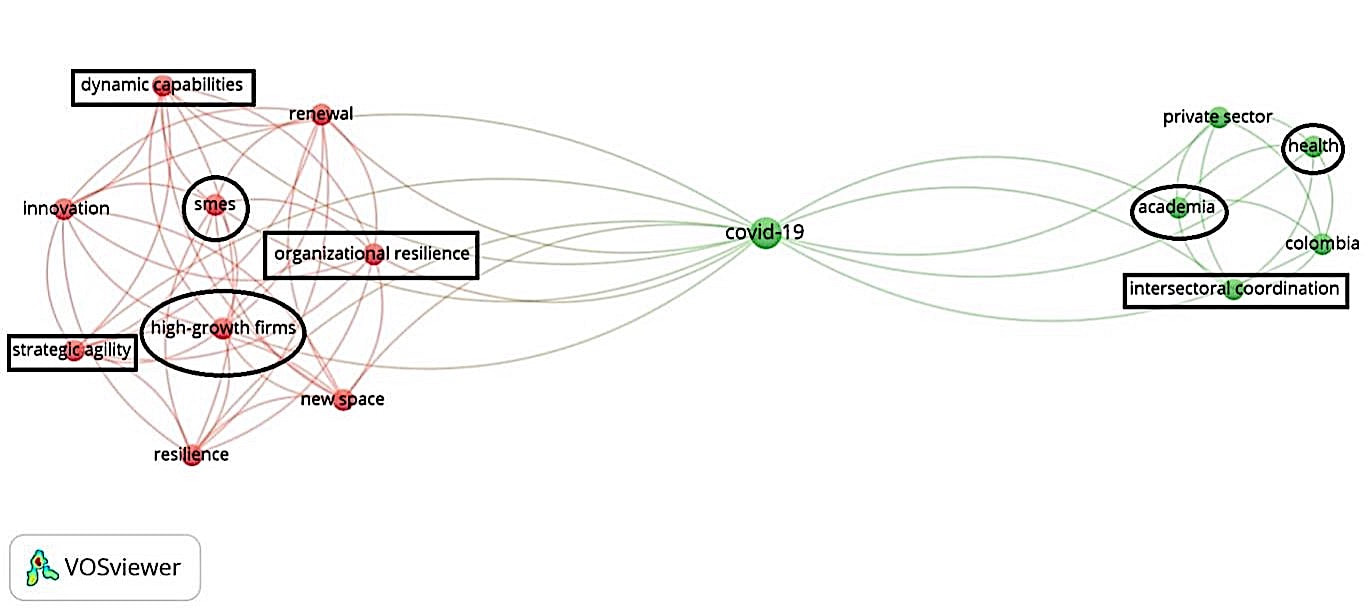
NeurologyPrevious studies have sought to evaluate the effects of space radiation on the human brain by delivering radiation doses to rodents over a few minutes. However, on missions to the Moon and Mars, powerful radiation will be gradually delivered to astronauts for the duration of the trip, ranging from weeks to years. A 2019 study from the journal eNeuro aims to more accurately simulate long-duration exposure by delivering low-level neutron radiation to mice for six months and evaluating the neurological implications. The study finds that exposure to cosmic rays impairs the brain function of the mice, affecting learning, memory, and mood. Lab tests reveal that following the neutron radiation, neurons are less responsive in the hippocampus - an area critical for the formation of memories and spatial navigation - and the medial prefrontal cortex - an area responsible for accessing preexisting memories, decision-making, and processing social information. Follow-up evaluations of the irradiated mice determine that neural circuitry damage may last for up to one year. Some researchers dispute the study’s approach, claiming that neutron radiation used in the experiment is not a viable surrogate for the galactic cosmic radiation that astronauts would encounter during deep space missions. Still, the eNeuro study offers a novel analogue to the gradual doses of powerful space radiation that astronauts would face on missions to the Moon and Mars, further emphasising the importance of effective shielding from cosmic rays. Researchers are also studying how microglia - the immune cells of the central nervous system - can be manipulated to prevent the development of cognitive deficits due to galactic cosmic ray exposure, a promising step toward protecting astronauts on deep space missions. ConclusionMotivated government leaders and entrepreneurs alike have expressed their commitment to bringing the human race beyond low Earth orbit. As breakthroughs in deep space research and aerospace technology bring this goal closer to realisation, concomitant advancements in space medicine must be made to safeguard astronauts’ health as they travel to and thrive in extraterrestrial environments. Before we can walk on Mars, our first step must be understanding and mitigating the health challenges that await us deeper into the final frontier. The term 'space sciences' is a conglomeration of almost all of the branches of science known to humanity today. Space fuels exploration and provides enormous opportunities for exploitation to meet societal needs. So much so that one finds the footprint of space technology in almost every aspect of daily life. For example, data received from earth observations help us to understand the global environmental factors and initiate ground-based measures to tackle them. Integrating data with fields like agriculture helped us develop 'Precision Agriculture'. Furthermore, space-driven initiatives drive international cooperation on issues related to humanity. Thus, it is pretty evident that any new crisis or breakthrough in almost any aspect of society will impact on the space industry. Such was the case when devastating waves of COVID-19 hit the world. Presented below is a bibliometric mindmap that gives us a visual aid to further our understanding of the true nature of the negative impact of the pandemic on the space industry. Figure: Impact of COVID-19 on the space industry and vice versa (Adopted with modifications from Palit S et al. - Space Industry and COVID-19: An Insight into Their Shared Relation) Note: Circles/ovals- Represent institutions affected by the COVID pandemic; Rectangles- Represent institutional values affected by the COVID pandemic It can be seen that the pandemic dealt a severe blow to institutions (such as SMEs, academia, the health sector) and their values (such as organisational resilience, etc.). However, as the saying goes, 'every cloud has a silver lining', and such was the case with COVID-19. Areas in which COVID-19 had positive implications include cases where:
Furthermore, astronauts onboard the International Space Station teach us some of the most valuable lessons. These include instances where the world applied containment measures to restrict the spread of pandemics, leading to the limited provision of healthcare resources. Here, the experiences gained with 3D printing during human spaceflights could help the healthcare industry to produce various tools (dental, medical, or surgical) and pharmaceutical products, and the list is endless.
Therefore, given the recent losses that we have suffered, it would be advisable to adopt space-based technologies as quickly as possible to help prevent the long-standing implications of COVID-19. However, this can only be done if we have collective support from government agencies worldwide. Author: Hamzah RahmanYear 3 student - Guy's, King's and St Thomas' School of Medicine & Space Enthusiast!  de Havilland Comet aircraft de Havilland Comet aircraft The General Practitioner (GP) medical professional has undoubtedly played a major role in providing a plethora of care packages and programmes for individuals seeking to travel; from immunisations and vaccinations to advice and even guidance for mothers in the late gestational stage. The advent of jet flight allowed the masses to venture to destinations that only aristocracy could once afford, which in turn generated a greater need for primary healthcare management. The GP is therefore the point of access to these healthcare packages and consequently plays a pivotal role in enabling tourists to travel safely. This responsibility is deeply intertwined with the historic increase in accessibility to affordable flight. The first British commercial jetliner was the de Havilland Comet in 1949. This aircraft enabled more people to travel further, as well as reducing the price of tickets substantially. The GP during this age would have played an important role in ensuring that passengers were fit to fly, by managing their pre-flight healthcare requirements.  Boeing 747-121 | Image credit: Aldo Bidini Boeing 747-121 | Image credit: Aldo Bidini The Boeing 707 soon joined the aviation world in 1957 and dramatically changed the way we travelled; it opened flight corridors that were once untenable, and consequently, accessed a greater consumer market - the working classes. In 1969, Boeing unveiled the revolutionary 747, coined the “Jumbo Jet” due to its sheer size, which resulted in greater passenger capacity and far more affordable tickets. With such quantum leaps forward in jet aviation, by the mid-70s the British GP was providing care and advice to thousands of travellers from all walks of life, different backgrounds and with all manner of pre-existing health conditions. The workload of the GP thus became much more diverse and they gained great responsibility in permitting the public to exercise their freedom to travel safely. Just as jet flight was once an exclusive mode of transport for those from higher socio-economic backgrounds, spaceflight has now emerged onto the world market with exclusive and expensive tickets to fly. Undoubtedly, spaceflight will become more affordable in the coming years and decades, and as such will inevitably require a more established initial healthcare access point for travellers- a service that GPs could provide. As space tourism flights become more accessible through lower prices and increased provision, the remit of travel healthcare provided by general practice could evolve in the near future to encompass spaceflight health clearance.
|
Welcometo the InnovaSpace Knowledge Station Categories
All
|
UK Office: 88 Tideslea Path, London, SE280LZ
Privacy Policy I Terms & Conditions
© 2024 InnovaSpace, All Rights Reserved













 RSS Feed
RSS Feed