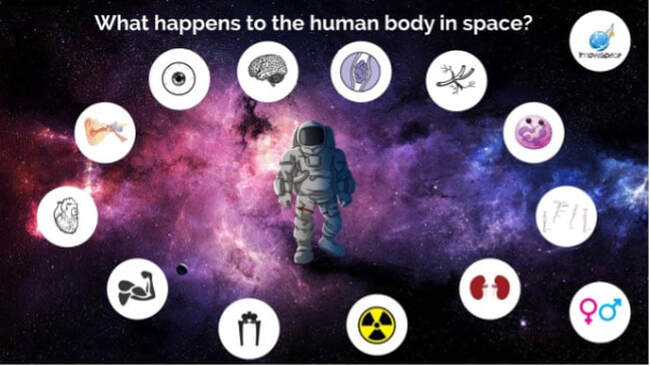
Author: Lucas RehnbergNHS Doctor - Anaesthetics & Intensive Care | MSc Space Physiology & Health  My name is Lucas, I am a doctor in the UK working in anaesthetics (or Anaesthesiology for any American readers) and intensive care medicine. I have had an interest in space medicine for over 10 years now, inspired by none other than Prof Thais Russomano who has mentored me over the years and still does. My Master’s dissertation (back in 2009) focused on CPR (cardiopulmonary resuscitation) methods in microgravity, with my continued research interest surrounding critical care in space. I am careful to say that I am a doctor with an interest in space medicine and physiology, as opposed to a ‘Space Doctor’ – as there are many individuals out there who have committed many more years than I have to this field and are vastly more experienced than I am! A club I aspire to join one day. The idea of this blog, or series of blogs, is to look at some of the latest research in space physiology and space medicine, then consider how this will play out clinically. With a particular focus on critical care and potentially worst-case scenarios when in space (or microgravity environment). Something all doctors will have done in their careers; we are equipped with the skills to critically appraise papers and then ask if they are clinically relevant, or how will it change current practice. Over the last 60 (ish) years of human space flight, there is lots of evidence to show that there are many risks when the human body has prolonged exposure to microgravity, which can affect most body systems – eyes, brain, neuro-vestibular, psychological, heart, muscle, bone, kidneys, immune system, vasculature, clotting and even some that we haven’t fully figured out yet. But then what needs to be done is to tease out how clinically relevant are these from the research, how could that potentially play out if you were the doctor in space, then how to mitigate that risk and potentially treat it. Space medicine is not lacking research, there are several space agencies (NASA, JAXA, ESA, Roscosmos) with multiple research groups, then there are international experts and groups that provide the international space community with vast and invaluable data. But, in general, this field is hampered by low numbers when it comes to data and sample sizes. If you compare it to terrestrial research, at the pinnacle of original research you can have a large multi-centred, randomised control trials that can have thousands of patients across several countries. Then you have a systematic review or meta-analysis that could pool tens of thousands of patients or data points, space medicine can’t even get close to these numbers.  Identical twins, Scott and Mark Kelly. Scott (L) spent a year in space while Mark (R) remained on Earth as control; researchers studied how the human body is affected by prolonged times spent in space. Credits: NASA Identical twins, Scott and Mark Kelly. Scott (L) spent a year in space while Mark (R) remained on Earth as control; researchers studied how the human body is affected by prolonged times spent in space. Credits: NASA So, when it comes to human physiology and space medicine research, you have to remember this. Like the Twin study done by the Kelly brothers – a truly unique study in space life sciences research and produced an incredible data set to be analysed, but ultimately there were only 2 subjects in that study. And even with the ISS being continuously active for the last 20 years, the sample sizes are still quite small (when compared to terrestrial medical research). It would be great to have larger sample sizes and we can partly achieve this by using ground based analogues, but we will simply never have the same size studies as we have in terrestrial medicine – as to date there have been fewer than 600 individuals who have flown in space (depending on your definition of space - STATS ) since 12th April 1961. That is not to say the research done to date isn’t incredible - as it is remarkable what all these international groups have achieved and contribute to the shared knowledge of space life sciences. All of this is what I find so interesting about space medicine, all these ‘unknowns’ of how the body is affected, how can we prevent it, how would we potentially treat it whilst onboard the ISS, on the Moon or several million miles away heading to Mars with no one else to help. Like in remote environments on Earth, like Antarctica research stations, there are limited resources in microgravity, but with even more isolation and remoteness to get back to a terrestrial hospital. In the ISS, an emergency evacuation can get you down in 6 hours, but think of that journey? Flying in a plane or helicopter can’t be comfortable if you have multiple injuries being flown into a trauma centre, but then think of being strapped inside a cramped Soyoz capsule with a fairly impressive G-force profile! Not to mention the challenge of monitoring and treating a critically unwell patient while in transit. Then take this a step further, how do we achieve critical care level medicine whilst ‘en route’ to Mars with limited resources and communication from Earth? To me, this is all incredibly fascinating!
This blog is inspired by some personalities on social media that I follow (like EddyjoeMD, @savinglivespodcast, Rishimd, icuexplained, The Bottom Line, Life in the fast lane, and many more, if you are interested in anaesthesia or critical care medicine) – so credit to all those individuals who share their expertise and experience in the name of #FOAMed. Comments are closed.
|
Welcometo the InnovaSpace Knowledge Station Categories
All
|
InnovaSpace Ltd - Registered in England & Wales - No. 11323249
UK Office: 88 Tideslea Path, London, SE280LZ
Privacy Policy I Terms & Conditions
© 2024 InnovaSpace, All Rights Reserved
UK Office: 88 Tideslea Path, London, SE280LZ
Privacy Policy I Terms & Conditions
© 2024 InnovaSpace, All Rights Reserved

 RSS Feed
RSS Feed